Peptides
- 5-amino-1MQ
- Aminophylline
- Aniracetam
- ARA 290
- Argireline + Leuphasyl
- BPC-157
- Bremelanotide
- Cerebrolysin
- CJC-1295
- Delta Sleep-Inducing Peptide
- Dihexa
- Elampretide (SS-31)
- Epithalon
- FG Loop Peptide (FGL)
- GHK-Cu
- Ginsenoside Rg3
- Glycyrrhetinic Acid
- Ipamorelin
- Kisspeptin
- KPV
- LL-37
- Melanotan 1
- Melanotan 2
- Mitochondrial ORF of the twelve S c (MOTS-c)
- MK-677 (IBUTAMOREN)
- Nicotinamide Adenine Dinucleotide (NAD+)
- Nicotinamide Riboside
- NMN (Nicotinamide Mononucleotide)
- Noopept
- Pegylated Mechano Growth Factor
- Selank
- Semax
- Sermorelin
- SRT2104
- Tesamorelin
- Thymosin Alpha 1
- Thymosin Beta 4
- Tiger 17
- Valproic Acid
- Valproic acid + PTD-DBM
- Vasoactive Intestinal Peptide
- Zinc-Thymulin
- Potential Health Benefits of Tesofensine
- Key Takeaways of Tesofensine Guide 2023
- What is Tesofensine?
- How Does Tesofensine Work?
- Chemical Structure of Tesofensine
- Research Studies on Tesofensine
- Associated Side Effects of Tesofensine
- Tesofensine Dosage
- Tesofensine vs Semaglutide
- Tesofensine Before and After Results
- FAQs
- Blog
- Reference
Table of Contents
- Potential Health Benefits of Tesofensine
- Key Takeaways of Tesofensine Guide 2023
- What is Tesofensine?
- How Does Tesofensine Work?
- Chemical Structure of Tesofensine
- Research Studies on Tesofensine
- Associated Side Effects of Tesofensine
- Tesofensine Dosage
- Tesofensine vs Semaglutide
- Tesofensine Before and After Results
- FAQs
- Blog
- Reference
Potential Health Benefits of Tesofensine
Tesofensine offers a range of potential benefits, including promoting weight loss, improving cognitive health, enhancing mood, regulating blood sugar levels, boosting energy, addressing sexual dysfunction, treating eating disorders, managing ADHD, improving sleep quality, and aiding in the fight against alcohol addiction.
- Promotes weight loss [6-23]
- Improves cognitive health [24-32]
- Improves mood [33-35]
- Improves blood sugar levels [36-38]
- Increases energy levels [35, 39]
- Treats sexual dysfunction [35, 40]
- Treats eating disorders [8, 41-45]
- Treats attention-deficit/hyperactivity disorder (ADHD) [46-49]
- Improves sleep quality [50-57]
- Fights alcohol addiction [58-62]
Key Takeaways of Tesofensine Guide 2023
- Tesofensine is a triple re-uptake inhibitor that increases the levels of three neurotransmitters in the brain: Serotonin, norepinephrine, and dopamine.
- Tesofensine benefits include weight loss, fat loss, increased energy levels, improved sex drive, better erections, improved mood, improved memory, improved concentration, better sleep, and better blood glucose levels by improving insulin sensitivity and glucose metabolism. Tesofensine causes a significant increase in weight loss and fat loss by reducing appetite, increasing resting energy expenditure (ie increasing metabolism and calories burned), increasing fat oxidation, and reducing fat tissue.
- Tesofensine is one of the most effective, powerful weight-loss medications available on the market. Studies have shown more weight loss with higher tesofensine doses was up to 1 mg. A clinical study found that participants receiving tesofensine at doses of 0.25 mg, 0.5 mg, and 1.0 mg in conjunction with a prescribed diet for 6 months had a mean weight loss of 4.5%, 9.2%, and 10.6%. Comparatively, patients in this study treated with a placebo only lost an average of 2% of their body weight. There was a 4-point drop in BMI in a period of 24 weeks in those treated with 0.5 mg and 1 mg.
- Tesofensine has been shown to have a good safety profile and was well tolerated although an increased number of adverse events (e.g., increased heart rate and blood pressure) were observed in the higher dose groups of 0.5 mg and 1.0 mg. Blood pressure and heart rate were increased by 1–3 mmHg and up to 8 bpm, respectively. Other side effects of Tesofensine may include dry mouth, headache, nausea, insomnia, diarrhea, and constipation. Although some studies show it may have anti-anxiety properties, some people may experience an increase in anxiety levels. Side effects are dose-dependent and are more significant when using higher doses.
- The tesofensine dosage range used in studies was 0.25 mg to 1 mg. The weight loss of 9.2% in the 0.5 mg tesofensine dose vs 10.6% in those using the 1 mg tesofensine dose may not justify the dose-dependent increases in side effects. Based on this, the best tesofensine dose for most patients would be 0.5 mg or lower. You should consult your weight loss expert doctor to determine if tesofensine is right for you and the dosage should be custom tailored.
- Only purchase tesofensine through a legally accredited US pharmacy prescribed by your expert weight loss doctor custom tailored for you. Do not buy tesofensine online because there are no testing requirements or regulations of these products to guarantee that it is even tesofensine, that is high-quality tesofensine, and that it is pure and does not contain any harmful chemicals. Consult with an expert weight loss doctor who has a lot of experience prescribing tesofensine and understands its potential side effects, contraindications, and drug interactions. A thorough medical history and exam should be completed along with the appropriate blood work. Caution: Tesofensine is a prescription medication that can cause side effects and it may not be a good weight loss option for you based on your medical history, blood work, or current medication use. An expert weight loss doctor will help you determine this. Tesofensine is not a supplement and should not be purchased online as a supplement. It is also very unwise for humans to use this medication by purchasing it online on websites that sell it with the legal loophole that it is being sold “for research purposes only”.
What is Tesofensine?
Tesofensine (NS2330) is a serotonin–noradrenaline–dopamine reuptake inhibitor or also known as a triple reuptake inhibitor, which means that it inhibits the reabsorption of the neurotransmitters (brain chemicals) serotonin, norepinephrine, and dopamine. This process increases the levels of these neurotransmitters. The therapeutic benefits of tesofensine are attributed to this effect because each of these neurotransmitters exerts an important function at different locations in the brain. Tesofensine peptide has been investigated in clinical trials for its use in medical weight loss.
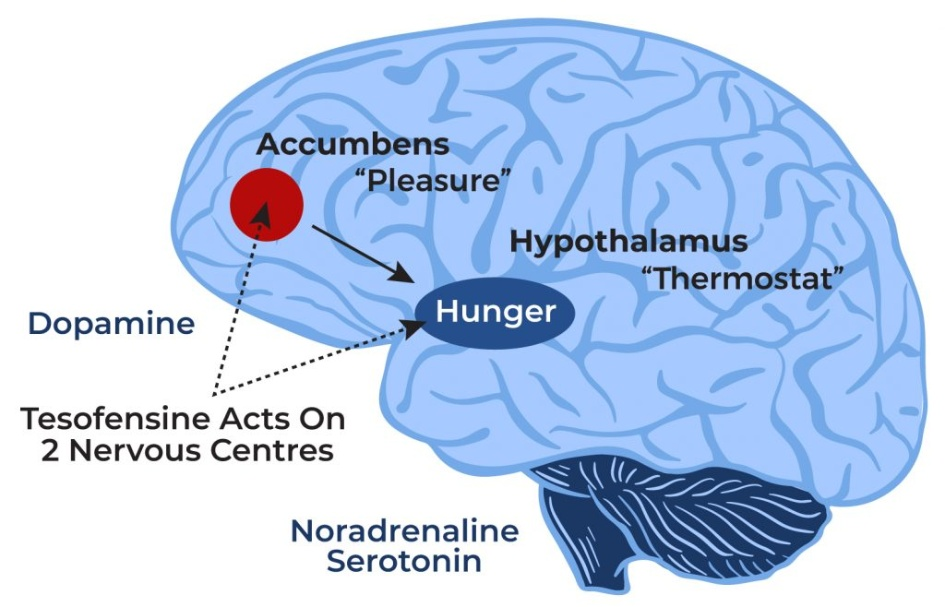
How Does Tesofensine Work?
Tesofensine works by boosting the levels of brain chemicals (neurotransmitters) such as dopamine, norepinephrine, and serotonin. Dopamine is associated with the regulation of motor function, mood, motivation, reward, cognitive function, and reproductive behaviors. Norepinephrine increases the force of the contraction of the skeletal muscle and the heart to ensure optimal body function. Serotonin is responsible for the regulation of mood, memory, sleep, and appetite.
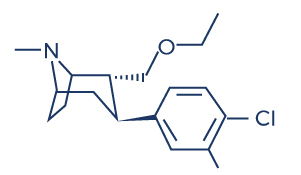
Chemical Structure of Tesofensine
Research Studies/Clinical Trials on Tesofensine
A. Promotes Weight Loss

Optimal dopamine levels have a positive impact on appetite regulation, metabolism, and motivation. On the other hand, dopamine deficiency can promote weight gain. Dopamine suppresses appetite, reduces cravings, and lowers calorie consumption. It also boosts metabolism by increasing thermogenesis, leading to improved calorie burning and increased energy expenditure. Moreover, dopamine enhances motivation and satisfaction, which helps produce feelings of satiety.
Tesofensine is widely known as a weight loss drug. Researchers believe that tesofensine may help treat obese and overweight patients because it boosts the levels of dopamine in the brain. A deficiency in this neurotransmitter has been shown to be linked with overeating and obesity. [1-5]
Fat oxidation, also known as lipid oxidation or fat burning, refers to the process by which stored fat is broken down and converted into usable energy within the body. There are some mechanisms by which tesofensine may contribute to increased fat burning such as increased metabolism, appetite suppression, and modulation of neurotransmitters. As an appetite suppressant, it may indirectly promote increased physical activity which leads to increased fat oxidation. When combined with lifestyle modification, the body responds well to the effects of tesofensine.
Discover the Power of Peptides for Weight Loss! Learn how peptides can support your weight loss journey and improve your overall health. Explore our comprehensive guide on peptides for weight loss at Genemedics and take the first step towards a healthier, happier you!
Clinical trials involving tesofensine have evaluated its efficacy and safety in promoting weight loss:
- The results of phase III trials such as the 2018 phase 3 Viking study showed that obese participants who received both doses of oral tesofensine (0.25 and 0.50 mg once daily) had statistically and clinically significant reductions in weight with low incidence of adverse events at week 24. [6]
- The results of clinical trials such as the Phase II b trial (TIPO-1) showed that obese patients lost an average of 12.8 kg on the 1 mg dose, 11.3 kg on the 0.5 mg dose, and 6.7 kg on the 0.25 mg dose of tesofensine (dose-dependent increase), and showed no statistically significant increases in systolic or diastolic blood pressure, compared with a 2.2 kg loss in the placebo group. [7] The 24-hour fat oxidation (fat burning) also increased by 15% and there was a reduction in protein oxidation (the breakdown of protein due to the presence of reactive oxygen species).
- In the TIPO-2 trial, tesofensine administration in obese individuals reduced their desire to eat and increased their satiety levels after 14 days of treatment. [8]
- In patients with obesity, tesofensine treatment at varying doses (0.25 mg, 0.5 mg, or 1.0 mg) resulted in statistically significant and clinically relevant weight reductions with positive effects on energy balance and appetite. The patients were also able to increase their physical activity gradually, which led to improved quality of life. Significant results were seen in the highest dose groups. [9]
- In obese participants, tesofensine administration at a dose of 0.5 mg for 26 weeks produced weight reductions twice that of anti-obesity agents such as sibutramine or rimonabant. [10]
- In overweight patients, tesofensine administration for 24 weeks is associated with enhanced appetite suppression and significant weight reductions. [11]
- In phase II clinical trials with tesofensine in obese individuals, significant reductions in weight, body fat, and waist circumference were observed without any adverse side effects. [12]
- In obese individuals, long-term tesofensine supplementation was well-tolerated and resulted in statistically significant and clinically relevant weight loss. [13]
- In patients with Parkinson’s or Alzheimer’s disease, tesofensine administration once daily for 14 weeks induced weight loss of approximately 4%, which is similar to that of sibutramine. [14]
- In healthy males, multiple administrations of tesofensine at doses of 0.125–1 mg resulted in the following positive results: increased dopamine levels and appetite suppression. [15]
- In diet-induced obese rats, tesofensine administration resulted in appetite suppression and weight loss with a reversal of low forebrain dopamine levels. [16-17]
- In a rat model of diet-induced obesity (DIO), administration of tesofensine (2.0 mg/kg, s.c.) for 16 days significantly reduced body weights. [18]
- In diet-induced obese rats, tesofensine treatment at 2 mg/kg for 28 days decreased food consumption and produced dramatic weight losses while preventing weight gain. [19]
- In 203 obese persons, tesofensine 0.5 mg produced a weight loss twice that of currently approved anti-obesity medications. [20]
- In obese participants, tesofensine administration resulted in a 10% average weight loss in 24 weeks. The patients were also able to increase their physical activity gradually after the treatment. [21]
- A study showed that tesofensine showed a more significant effect on body weight than that of currently approved anti-obesity drugs. [22]
- In obese patients, tesofensine in combination with an energy-restricted diet effectively reduced the weight of the subjects. [23]
B. Improves Cognitive Health

Research indicates that tesofensine helps preserve cognitive health by indirectly potentiating cholinergic neurotransmission, which is a process whereby nerve cells relay messages to each other. [24] This has been proven to have beneficial effects on various areas in the central nervous system and cognitive health including learning, memory, and thinking skills. This suggests that tesofensine may be used in the treatment of brain disorders such as Alzheimer’s and Parkinson’s disease. The following studies support this effect:
- The first results of two small 4-week phase IIa clinical trials performed in patients with mild Alzheimer’s disease (AD) showed that tesofensine treatment induced significant improvement in cognitive function, indicating the need for phase III trials. [25-26]
- A growing body of research indicates that obesity is a major risk factor for cognitive impairment, especially in the older population. [27-30] With its anti-obesity effect, tesofensine may help protect against cognitive impairment.
- In a mouse model of Alzheimer’s disease, tesofensine administration decreased the brain concentrations of amyloid beta, which are abnormal protein aggregates and is the causative agent of the disease. [31]
- In patients with advanced Parkinson’s disease and motor fluctuations, low-dose tesofensine improved activities of daily living and motor function. [32]
C. Improves Mood

The mood centers of the central nervous system have also been shown to be positively affected by tesofensine. Sustained treatment with tesofensine has been shown to improve overall mood through its antidepressant effect. Studies show that tesofensine affects mood by:
- Increasing the levels of brain-derived neurotrophic factor (BDNF), thereby triggering an antidepressant effect. [33]
- Triggering an anti-anxiety effect in obese individuals with comorbid depression and anxiety symptoms. [34]
- Increasing the levels of the neurotransmitters serotonin, noradrenaline, and dopamine. [35]
D. Improves Blood Sugar Levels

Tesofensine has also been found to have beneficial effects on blood sugar. By promoting weight loss, tesofensine may indirectly contribute to improving insulin sensitivity in individuals with obesity or overweight. Insulin sensitivity refers to the body’s ability to respond to the effects of insulin, a hormone that acts as a key to unlocking cells, thus allowing glucose (blood sugar) from the bloodstream to enter and be utilized by cells for energy production. Weight loss also plays a significant role in reducing blood sugar levels and decreasing the incidence of type II diabetes.
Clinical trials have shown that weight loss drugs such as tesofensine demonstrate efficacy in improving blood sugar levels:
- In obese patients, administration of tesofensine at varying doses (0.25 mg, 0.5 mg, and 1.0 mg) resulted in a reduction in blood sugar levels and improvement in quality of life with significant results observed in the highest dose groups. [36]
- In rodents, tesofensine also induced a significant reduction in blood sugar levels in addition to weight loss. [37-38]
E. Increases Energy Levels

Tesofensine treatment is also beneficial in improving one’s productivity by increasing energy levels. Medical weight loss programs with this medication can cause a significant increase in energy levels by having the following positive results: reduced appetite with balanced nutrition, increased physical activity, increased metabolism resulting in more calories being burned, and hormonal balance. Evidence supports the energy-boosting effects of tesofensine:
- A study found that tesofensine can boost energy by increasing the levels of the neurotransmitters dopamine and norepinephrine, which help regulate energy balance, motivation, interest, and drive. [35]
- The administration of tesofensine in overweight and moderately obese men induced higher energy expenditure compared to placebo. [39]
F. Treats Sexual Dysfunction

Because of its potent antidepressant effect, tesofensine has also been studied for its therapeutic benefits on sexual dysfunction, according to studies:
- Tesofensine has the capacity to increase the levels of dopamine, a neurotransmitter that contributes to the desire for sexual activity, erection, and ejaculation, making it beneficial for patients with sexual dysfunction related to dopamine deficiency. [35]
- Tesofensine administration is effective in treating depression-related sexual dysfunction, suggesting that it can help ramp up sexual power. [40]
G. Treats Eating Disorders

Studies reported that triple reuptake inhibitor such as tesofensine also holds therapeutic potential for eating disorders:
- In obese patients, tesofensine administration reduced their desire to eat and resulted in a significant increase in their satiety levels after 14 days of treatment without adverse events. [8]
- In patients with binge eating disorder, a condition in which a person eats large quantities of food when stressed, tesofensine administration has been shown to improve its symptoms, possibly due to tesofensine’s potent antidepressant effect, without an adverse event. [41-44]
- In the diet-induced obese rat, tesofensine induced appetite suppression by indirect stimulation of α1 adrenoceptor and dopamine d1 receptor pathways. [45]
H. Treats Attention-Deficit/Hyperactivity Disorder (ADHD)

ADHD is characterized by short attention span, hyperactivity, and impulsivity, and is common in children and even adults. Evidence suggests that tesofensine may have beneficial effects on this mental condition:
- Studies show that ADHD is strongly linked with low levels of dopamine and serotonin and that tesofensine can have beneficial effects on this condition by increasing the levels of these neurotransmitters. [46-48]
- A study reported that tesofensine can lower the risk of ADHD associated with obesity. [49]
I. Improves Sleep Quality

Studies suggest that tesofensine’s ability to increase the levels of certain neurotransmitters can help improve sleep quality:
- A deficiency in the neurotransmitter serotonin has been linked to insomnia and various sleeping difficulties. [50-55]
- Studies reported that increasing the levels of serotonin through selective serotonin reuptake inhibitor treatment has been shown to improve objective and subjective sleep quality in patients with sleeping difficulties – an effect similar to tesofensine. [56-57]
J. Fights Alcohol Addiction
Neurotransmitters play a significant role in alcohol addiction. Alcohol affects several neurotransmitter systems in the brain, leading to the addictive and rewarding effects associated with alcohol consumption. There’s also evidence suggesting that tesofensine can cure alcohol addiction via its ability to boost neurotransmitter levels:
- Studies show that low dopamine levels are associated with alcohol addiction – with tesofensine’s ability to increase dopamine levels, it may help reduce excessive alcohol intake along with its symptoms. [58-61]
- In ethanol-preferring rats, triple reuptake inhibitor administration reduced alcohol consumption without decreasing food or water consumption. [62]
Associated Side Effects of Tesofensine
Tesofensine side effects are very uncommon and similar to other currently approved diet pills and weight loss medications. There have been some side effects associated with the use of this drug wherein the patient had one of the issues listed below at some point while being on tesofensine. However, these side effects weren’t confirmed to be associated with the treatment and could have been a coincidence and not related to the use of tesofensine. Despite this, it was listed as a side effect associated with tesofensine even though these associated side effects are very uncommon.
Side effects associated with tesofensine may include the following:
- Constipation
- Diarrhea
- Dry mouth
- Headache
- Changes in blood pressure (increase blood pressure)
- Increased heart rate
- Insomnia
- Nausea
Tesofensine Dosage
Studies have indicated that the tesofensine dosage range employed was between 0.25 mg to 1 mg. However, the weight loss achieved with a 0.5 mg dose (9.2%) was only slightly lower than that of a 1 mg dose (10.6%). Considering the dose-dependent rise in side effects, it raises questions about the justifiability of higher doses.
Based on this information, for most patients, a tesofensine dose of 0.5 mg or lower appears to be the most suitable option. However, it is crucial to consult with your weight loss expert doctor to assess if tesofensine is appropriate for your specific circumstances and to determine the optimal dosage tailored to your needs.
The dosage of tesofensine is determined on an individual basis, taking into consideration various factors such as health conditions and medical history. It is important to note that not everyone may be eligible for tesofensine treatment due to specific health issues. Therefore, individuals are strongly advised to consult with a qualified tesofensine doctor or healthcare professional who has expertise in prescribing tesofensine. Seeking guidance from an expert will help ensure that tesofensine is prescribed in a safe and appropriate manner, tailored to the specific needs and circumstances of each individual.
Tesofensine vs Semaglutide
Tesofensine and semaglutide are both medications that have shown potential for weight loss in clinical trials, but they differ in their mechanisms of action and approved uses.
- Mechanisms of Action: Tesofensine is an inhibitor of pre-synaptic uptake of the neurotransmitters serotonin, noradrenaline, and dopamine. This causes appetite suppression and produces feelings of satiety. Semaglutide, on the other hand, is a glucagon-like peptide-1 (GLP-1) receptor agonist. It works by mimicking the action of a naturally occurring hormone called GLP-1, which helps regulate blood sugar levels and reduce appetite.
- Approved uses: Tesofensine is used for the treatment of obesity. On the other hand, semaglutide is an approved medication used for type 2 diabetes and obesity.
Tesofensine Before and After Results
About Dr. George Shanlikian
Dr. George Shanlikian, renowned as the world’s best hormone therapy doctor, possesses expertise in various medical domains. These include Bioidentical Hormone Replacement Therapy, Peptide Replacement Therapy, Anti-Aging Medicine, Regenerative Medicine, Stress Management, Nutrition Consulting, Nutritional Supplement Consulting, and Exercise Consulting.
Read more about him here: https://www.genemedics.com/dr-george-shanlikian-md-best-hormone-therapy-doctor
Read more success stories here:
Men’s Success Stories: https://www.genemedics.com/about-ghi/ghi-success-stories/mens-success-stories/
Women’s Success Stories: https://www.genemedics.com/about-ghi/ghi-success-stories/womens-success-stories/
FAQ
Does tesofensine work for weight loss?
Tesofensine, a promising weight loss medication, has regularly faced pharmacovigilance hurdles during its drug development and clinical trials. However, it has shown promising results for weight loss in early clinical trials. Several studies have assessed the effects of tesofensine on weight reduction and have reported positive outcomes. For instance, a phase II trial assessed the weight loss properties of tesofensine in obese patients and found significant reductions in body weight and visceral fat. [7]
What does tesofensine do?
Tesofensine, a presynaptic serotonin–noradrenaline–dopamine reuptake inhibitor, suppresses appetite, reduces food cravings, and helps produce feelings of satiety by affecting neurotransmitter levels in the central nervous system. This in turn decreases caloric intake. In addition, it enhances thermogenesis (the process by which the body generates heat and burns calories), resulting in increased energy expenditure and decreased fat.
How much weight can you lose on tesofensine?
The amount of weight and fat tissue that can be lost with tesofensine can vary among individuals, and it depends on several factors including initial body weight, overall health, lifestyle habits, and adherence to a calorie-controlled diet and exercise regimen.
How much tesofensine should I take?
Just like other weight loss medications, the dosage of tesofensine should be determined and prescribed by a qualified healthcare professional to avoid adverse effects. The appropriate dosage may vary depending on several factors, including your individual health condition, weight loss goals, and potential interactions with other medications or medical conditions.
What are the risks of taking tesofensine?
Common side effects include dry mouth, headache, nausea, insomnia, diarrhea, and constipation. It may also increase systolic or diastolic bp. To avoid any repetition of drug scandals related to anti-obesity drugs, tesofensine should be carefully monitored and thoroughly studied for its effectiveness and safety in treating weight-related conditions.
How long does it take for tesofensine to work?
The timeframe for tesofensine to take effect can vary from person to person. The exact timeline may depend on factors such as individual metabolism, adherence to a prescribed diet and exercise regimen, and the specific dosage of tesofensine being used.
How often do you take tesofensine?
The frequency of tesofensine intake is determined by a healthcare professional.
Does tesofensine give you energy?
As an inhibitor of pre-synaptic uptake of the neurotransmitters serotonin, noradrenaline, and dopamine, it helps lose weight by suppressing appetite and increasing resting energy expenditure (your basal metabolic rate). Losing excess weight and adopting a healthier lifestyle can lead to increased energy levels and improved overall well-being.
Does tesofensine burn fat?
A clinical trial found that tesofensine increased satiety, sense of fullness, and 24-h fat oxidation (fat burning) in overweight and obese individuals. [7]
Is tesofensine addictive?
A study evaluated the potential abuse-related effects of tesofensine in recreational stimulant users and found that it is unlikely to be recreationally abused. [63]
Is tesofensine FDA approved?
The FDA has given special recognition to an experimental treatment for a condition called hypothalamic obesity. The treatment, called Tesomet, is a combination of two drugs: tesofensine, which affects certain brain chemicals, and metoprolol, which is a type of medication that targets the heart. This designation from the FDA means that the treatment will receive extra support and incentives to help it progress in its development and potentially become available to patients.
Is tesofensine an antidepressant?
Tesofensine exerts its antidepressant effects by increasing the levels of brain-derived neurotrophic factor (BDNF), serotonin, noradrenaline, and dopamine.
What is the half life of tesofensine?
Tesofensine stays in the body for about 8 days in humans and has the ability to raise dopamine levels in a stable way without sudden changes.
How much weight loss is produced by tesofensine in patients with Parkinson's or Alzheimer's disease?
Tesofensine can produce a weight loss of approximately 4% for >14 weeks without any diet and lifestyle therapy in this patient population.
Can you take tesofensine while pregnant?
Pregnant or breastfeeding women and individuals with uncontrolled high blood pressure should avoid taking tesofensine.
Is tesofensine a MAOI?
Tesofensine is a triple monoamine reuptake inhibitor. It works by blocking the reuptake of certain chemicals in the brain called monoamines. These chemicals include dopamine, norepinephrine, and serotonin, which are involved in various processes such as mood regulation, appetite control, and energy levels. By inhibiting their reuptake, tesofensine increases the levels of these chemicals in the brain.
Where can I buy tesofensine?
To ensure your safety and obtain genuine, high-quality tesofensine, it is crucial to only acquire it from a legally accredited US pharmacy, as prescribed by your expert weight loss doctor. They will tailor the prescription specifically for you, taking into account your unique needs.
How to take tesofensine?
The dosage and administration of tesofensine should be determined by a healthcare professional.
Does tesofensine work?
Tesofensine has shown promise in clinical trials for its potential effectiveness in promoting weight loss. In these trials, tesofensine has been associated with significant weight loss compared to placebo, and it has demonstrated effects on appetite suppression, increased metabolism, and fat oxidation.
When to take tesofensine?
The timing of tesofensine administration should be determined by a healthcare professional.
How long does tesofensine take to work?
The timeframe for tesofensine to take effect can vary and is typically determined by clinical trials and medical research. Therefore, the specific duration for tesofensine to produce noticeable effects is not well-established. During clinical trials, the effects of tesofensine are typically assessed over a specific period of time, often several weeks or months, to evaluate its effectiveness for the intended purpose. It’s important to note that individual responses to medications can vary, and some individuals may experience effects sooner or later than others.
Is tesofensine a peptide?
Tesofensine is a peptide that has been studied for its potential effects on weight loss, cognitive function, and other medical conditions.
Discover the Power of Wound Healing Peptides! Explore our collection of advanced peptides for faster and more effective wound healing at Genemedics. From collagen synthesis to tissue repair, our selection of peptides is designed to support your body’s natural healing process.
What is tesofensine used for?
Tesofensine is used to achieve medical weight loss in obese and overweight patients. It can help produce weight loss especially in individuals who are not responding to traditional methods such as diet and exercise.
What time of day to take tesofensine?
The specific time of day to take tesofensine would depend on the instructions provided by the prescribing physician or healthcare professional. They will consider various factors such as the individual’s medical condition, other medications being taken, and any specific considerations for optimal dosing.
Is it safe to take an appetite suppressant?
The safety of appetite suppressants depends on various factors, including specific medication, individual health conditions, and proper usage. It’s important to note that appetite suppressants can come in different forms and have different mechanisms of action. Some appetite suppressants are available as prescription medications, while others may be sold over the counter as dietary supplements. Prescription appetite suppressants are typically regulated and monitored by healthcare professionals. They may be prescribed for short-term use in individuals with obesity or weight-related health conditions. These medications are meant to be used under medical supervision and as part of a comprehensive weight management program.
What is the risk of appetite suppressants?
The use of appetite suppressants carries certain risks and potential side effects. These can include increased heart rate, elevated blood pressure, insomnia (sleeping problems), dry mouth, gastrointestinal issues, and the potential for misuse or dependence. Additionally, some appetite suppressants may interact with other medications or have contraindications for individuals with certain health conditions. Therefore, it is crucial to consult with a healthcare professional before using appetite suppressants, as they can assess your specific health situation, weigh the potential risks against benefits, and provide appropriate guidance to ensure safe usage.
What are the side effects of Tesomet?
The most common side effects of this medication are sleep disturbances, dry mouth, headache, and dizziness.
How long does an appetite suppressant last?
The duration for which these medications remain in the body can vary from individual to individual. While some people may experience the effects of the medication dissipating shortly after their last dose, others may notice effects lingering for up to 24 hours. However, in most cases, the effects typically diminish within a few days.
Does starving lower heart rate?
When you go without eating for a long time, your body goes through changes to protect itself. One of these changes is a slower heartbeat, which means your heart beats fewer than 60 times in a minute. This is called bradycardia. It’s a natural response to help prevent the breakdown of muscles and tissues when you’re not getting enough food.
Is peptide an appetite suppressant?
Peptides can potentially act as appetite suppressants, but it depends on the specific peptide and its mechanism of action. Peptides are short chains of amino acids that can have various effects on the body, including regulating appetite and metabolism. Some peptides, such as peptide YY (PYY) and glucagon-like peptide-1 (GLP-1), are known to have appetite-suppressing effects by signaling to the brain that you are full or by delaying gastric emptying. Peptide-based medications or treatments targeting appetite regulation have been studied in the field of obesity and weight management. These peptides may be administered through injections, infusions, or other delivery methods. However, it’s important to note that not all peptides are used as appetite suppressants, and the use of specific peptide-based medications would depend on factors such as prescription requirements and individual health conditions.
What are the effects of weight loss drugs?
Some people may experience symptoms like nausea, vomiting, diarrhea, or constipation when taking the medication. It is recommended to start with a low dose and gradually increase it to the desired level. Studies have shown that these side effects, such as diarrhea and nausea, are usually temporary and tend to go away on their own.
Are weight loss drugs effective?
These medications can assist individuals in losing 5% to 10% of their body weight, which can lower the risk of cardiovascular disease in adults who are overweight or have obesity.
Why do weight loss drugs work?
In recent years, the FDA has given approval to several medications for treating obesity, which aids in managing appetite and reducing food cravings. These weight loss drugs work by decreasing hunger, leading to a reduction in the number of calories consumed each day. Over time, consuming fewer calories results in weight loss.
What are the benefits of slimming?
Losing even a small amount of weight can have significant advantages, including better blood pressure, blood cholesterol, and blood sugar levels. This modest weight reduction can lower your risk for obesity-related chronic diseases.
Do I take an appetite suppressant on an empty stomach?
The specific instructions for taking an appetite suppressant can vary depending on the medication and the guidance provided by your healthcare professional. In some cases, appetite suppressants may be recommended to be taken on an empty stomach, while in other cases, they may be taken with food. It is important to carefully read and follow the instructions provided with the medication, including any recommendations regarding whether to take it on an empty stomach or with food. Additionally, it is advisable to consult with your healthcare professional or pharmacist for personalized advice on the best way to take the specific appetite suppressant prescribed to you.
What happens when you stop appetite suppressants?
When individuals discontinue the medication, they may observe a return to their pre-medication appetite levels. In certain instances, their appetites might even feel larger than they were prior to weight loss.
How safe is tesofensine?
It’s important to note that the safety of a medication can vary from person to person, and individual factors such as overall health, medical history, and potential interactions with other medications can influence its safety and tolerability.
How does tesofensine make you feel?
Tesofensine acts by affecting three brain chemicals: noradrenaline, serotonin, and dopamine, which play a role in controlling hunger. By taking this pill, individuals experience reduced hunger and a significant increase in the feeling of fullness, allowing them to eat less.
Are appetite suppressants healthy?
The healthiness of appetite suppressants depends on various factors, including specific medication, individual health conditions, and proper usage. It is important to note that appetite suppressants can have both potential benefits and risks. When used under the guidance of a healthcare professional and as part of a comprehensive weight management plan, prescription appetite suppressants may help some individuals with obesity or weight-related health conditions to reduce caloric intake and support weight loss efforts. They are typically prescribed for short-term use and monitored closely by healthcare professionals.
What time of day should I take my appetite suppressant?
The specific time of day to take an appetite suppressant can vary depending on the medication and the instructions provided by your healthcare professional. It is important to carefully read and follow the instructions provided with the medication. In some cases, appetite suppressants may be recommended to be taken in the morning to help control hunger throughout the day. This timing can be beneficial as it allows the medication to take effect when you may need the most support in managing your appetite. However, it is important to consult with your healthcare professional or pharmacist for personalized advice on the best time to take your specific appetite suppressant. They will consider factors such as the medication’s formulation, potential interactions with other medications, and your individual health needs to provide you with the most accurate guidance on when to take the medication for optimal effectiveness and safety.
Does hunger affect blood pressure?
Yes, hunger can potentially affect blood pressure. When you’re hungry, your body may experience changes in blood pressure levels. These changes can vary among individuals. In some cases, hunger can lead to a temporary increase in blood pressure. This is believed to occur as a result of the body’s stress response to the need for nourishment. During this response, stress hormones like cortisol and adrenaline are released, which can cause a temporary rise in blood pressure. Conversely, prolonged fasting or very low-calorie diets can sometimes lead to a drop in blood pressure. This may be due to a decrease in blood volume and a lower overall metabolic rate. It’s worth noting that the impact of hunger on blood pressure can be influenced by various factors such as individual physiology, overall health, and existing conditions like hypertension.
Does starvation affect blood pressure?
Yes, starvation can potentially affect blood pressure. Hunger can lead to a temporary increase in blood pressure while prolonged fasting or very low-calorie diets can sometimes lead to a drop in blood pressure.
What are the side effects of using peptides?
Some reported side effects of peptides may include water retention, numbness in the hands and feet, and increased fatigue.
How long do peptides take to work?
Peptide therapy typically requires a “loading” period of 3-6 months for the full effects to become noticeable. However, benefits can start appearing within the first few weeks and continue to improve with ongoing therapy. It is common during this period to use a combination of different peptides to maximize the desired outcomes.
What are the disadvantages of weight loss pills?
Weight loss pills can have several disadvantages. Firstly, they may come with side effects such as nausea, diarrhea, constipation, and gastrointestinal discomfort. Additionally, some weight loss pills can potentially interact with other medications, leading to adverse effects. Moreover, there is a risk of developing tolerance or dependence on weight loss pills, which may result in reduced efficacy over time or difficulty in maintaining weight loss once the medication is discontinued. Lastly, weight loss pills are not a magic solution and should always be used in conjunction with a balanced diet, regular exercise, and healthy lifestyle habits for sustainable weight loss. It is crucial to consult with a healthcare professional before using weight loss pills to understand the potential disadvantages and determine if they are suitable for your specific circumstances.
Why take peptides on an empty stomach?
Peptides are sometimes recommended to be taken on an empty stomach to optimize their absorption and effectiveness. When taken on an empty stomach, peptides can be absorbed more efficiently into the bloodstream as they are less likely to compete with other nutrients or substances in the digestive system.
What peptide kills appetite?
Peptides aid in weight loss by enhancing feelings of fullness and promoting muscle growth. Various peptides designed for weight loss, such as growth hormone secretagogues and receptor agonists, work by boosting the body’s metabolism of food and nutrients. These weight-loss peptides are available in both injectable and oral forms.
Discover the Power of Growth Hormone Boosting Peptides! Unlock your body’s full potential with our top-notch growth hormone-boosting peptides. Learn how these peptides can optimize your health and fitness goals.
Do peptides burn belly fat?
Peptides can potentially contribute to fat loss, including the reduction of belly fat. Certain peptides have been studied for their effects on fat metabolism and body composition. For example, peptides like growth hormone secretagogues and certain receptor agonists have shown potential in promoting fat-burning and improving body composition. However, it’s important to note that the effectiveness of peptides in burning belly fat can vary among individuals, and results may depend on various factors, including the specific peptide used, dosage, duration of use, overall lifestyle, and individual metabolism. Peptides alone are not a magic solution for spot reduction of belly fat. They should be used in conjunction with a balanced diet, regular exercise, and a healthy lifestyle to achieve the best results. It’s always recommended to consult with a healthcare professional or specialist experienced in peptide therapy for personalized advice based on your specific situation.
Are peptides for weight loss safe?
Peptides for weight loss can be safe when used under the guidance of a healthcare professional and in accordance with proper dosing and administration protocols. However, it’s important to note that the safety of peptides can vary depending on the specific peptide, dosage, individual health conditions, and how they are used.
What are the common side effects of weight loss drugs?
Weight loss drugs can have several common side effects. These may include an increase in blood pressure and heart rate, difficulties with sleep such as insomnia, feelings of nervousness and restlessness, and the potential for dependence, abuse, or withdrawal symptoms with prolonged use. It’s important to be aware of these potential side effects and consult with a healthcare professional when considering the use of weight loss drugs.
Does fat affect medication absorption?
Yes, the presence of dietary fat can affect the absorption of certain medications. Some medications require the presence of fat for optimal absorption, while others may have reduced absorption in the presence of high-fat meals.
How can I improve my fat digestion and absorption?
To improve fat digestion and absorption, you can focus on a few key strategies. Firstly, ensure you have adequate production and release of digestive enzymes, such as lipase, which help break down fats. This can be supported by consuming a balanced diet that includes healthy fats and avoiding excessive consumption of processed or high-fat foods. Additionally, optimizing your gut health through the consumption of probiotic-rich foods or supplements can enhance fat absorption. Lastly, be mindful of any underlying conditions that may affect fat digestion, such as pancreatic insufficiency or gallbladder dysfunction, and seek appropriate medical advice and treatment if necessary.
What are the short-term effects of weight loss drugs?
The short-term effects of weight loss drugs can vary depending on the specific medication. Generally, weight loss drugs may lead to reduced appetite, increased feelings of fullness, and a potential initial decrease in body weight. Some medications may also have stimulant properties, leading to increased energy levels and potential improvements in mood or focus. However, it’s important to note that individual responses can differ, and side effects may occur, such as nausea, gastrointestinal discomfort, dry mouth, or changes in bowel movements. Short-term effects should be monitored closely, and it’s crucial to follow the prescribed dosage and guidelines provided by a healthcare professional.
Why do people take weight loss drugs?
People may take weight loss drugs to assist with their weight management efforts. Weight loss medications may be prescribed to individuals with obesity or too much weight who have been diagnosed with medical conditions. These medications can help suppress appetite, increase feelings of fullness, or inhibit the absorption of dietary fat. They are intended to be used in conjunction with a balanced diet, regular physical activity, and lifestyle modifications. Weight loss drugs may be considered when other methods have not resulted in sufficient weight loss or when there is a need to address weight-related health concerns. It is important to note that the decision to take weight loss drugs should be made in consultation with a healthcare professional.
Do weight loss drugs work long-term?
The long-term effectiveness of weight loss drugs can vary depending on the specific medication, individual factors, and lifestyle habits. Weight loss drugs are typically prescribed for short-term or intermittent use and are intended to be part of a comprehensive weight management plan that includes a balanced diet, regular physical activity, and behavioral changes. While weight loss drugs can provide initial benefits in terms of appetite suppression and initial weight reduction, their long-term effectiveness may vary. Research suggests that weight loss achieved with medication alone tends to be modest, and individuals may regain weight once the medication is discontinued or if lifestyle changes are not maintained. Sustainable long-term weight loss and weight maintenance usually require adopting healthy eating habits, regular physical activity, and addressing underlying factors contributing to weight gain.
Does weight affect drug effectiveness?
Fluctuations in body weight can impact the dosage requirements and metabolism of medication within the body. When body weight changes, the circulatory system may be affected, potentially altering the rate at which drugs are transported to the liver and kidneys for processing. These factors can influence the speed at which medications are absorbed, distributed, and eliminated, necessitating adjustments to dosage regimens to ensure optimal effectiveness and safety.
How long does it take to lose weight?
In general, a realistic rate of weight loss for most individuals is about 1-2 pounds per week. However, it’s important to consider that everyone’s starting point and circumstances are different. A more effective benchmark to follow is aiming for 1-2% of your current weight as a guideline for your weight loss journey. By maintaining this percentage throughout your diet, the amount you expect to lose will gradually adjust in alignment with your evolving, lighter body weight. This approach allows for a more personalized and sustainable weight loss trajectory tailored to your individual needs.
What are the effects of losing body fat?
Losing body fat can have a range of positive effects on both physical and mental well-being. Physically, reducing body fat can lead to improved cardiovascular health, lowered blood pressure, decreased risk of chronic diseases such as diabetes and certain cancers, improved mobility and joint health, and increased energy levels. Additionally, losing body fat can enhance body composition by increasing lean muscle mass and improving overall body shape and definition. From a mental standpoint, weight loss can boost self-esteem, body image, and confidence, leading to improved mental health and a positive outlook. It’s important to approach weight loss in a balanced and healthy manner, focusing on sustainable habits that support long-term well-being.
How do you know if weight loss is permanent?
Determining if weight loss is permanent requires long-term maintenance of healthy habits and lifestyle changes. Sustained weight loss is more likely when individuals adopt a balanced and nutritious diet, engage in regular physical activity, and make sustainable behavioral modifications. It is important to recognize that weight maintenance is a lifelong process, and vigilance is needed to prevent weight regain. If individuals can maintain their healthier habits and weight over an extended period, it suggests that their weight loss is more likely to be permanent.
What happens if you take fat burners without working out?
If you take fat burners without engaging in regular physical exercise, the effectiveness of the fat burners may be compromised, and the desired results may not be achieved. Fat burners are typically designed to enhance weight loss by increasing metabolism, suppressing appetite, or promoting fat oxidation. However, exercise plays a crucial role in maximizing the benefits of fat burners.
Blog

Discover the Benefits of Tesofensine – Improve Your Health and Fitness
Introduction:
Are you looking for a reliable and effective way to improve your health and fitness? Then, a Tesofensine supplement might just be the answer you’re looking for. Tesofensine is a potent medication that stimulates your body’s metabolic rate and increases your energy levels. In this blog post, we’ll explore the benefits of Tesofensine and how it can help you achieve your health and fitness goals. So, let’s get started!
Increases Your Metabolic Rate
Tesofensine is a medication that increases your metabolic rate. It works by speeding up the process of converting the calories you consume into energy for your body to use. This results in a significant reduction of fat storage, which is particularly helpful in weight-loss management. With Tesofensine, you will begin to experience a gradual weight loss that’s much easier to maintain.
Enhances Your Energy Levels
Do you feel sluggish and tired most of the time? Tesofensine might just be the energy boost you need. It acts as a stimulant for your body, increasing your energy levels without causing the jitters or crash that come with caffeine or other stimulants. With more energy, you can work out more efficiently and complete your daily tasks with ease.
Reduces Your Appetite
One of the greatest benefits of Tesofensine is its ability to suppress your appetite effectively. It does this by regulating the hormones that cause hunger, making you feel full after eating much less food than you’re accustomed to. This leads to calorie restriction, which is vital in any weight loss or maintenance program.
Improves Your Mood
Tesofensine also has a subtle effect on your mood, making you feel more positive, upbeat, and motivated. With increased motivation and a positive frame of mind, you are better equipped to stick to your workout plans and healthy eating habits.
Supports Heart Health
Tesofensine is known to promote heart health by boosting blood circulation in the body. With improved circulation, your heart functions better, and your blood helps to nourish your vital organs effectively. It also reduces the risk of heart attacks, heart disease, and related conditions.
Conclusion:
In conclusion, Tesofensine is an excellent supplement to add to your health and fitness routine. Its numerous benefits make it an excellent choice for anyone who wants to maintain a healthy weight, boost energy levels, and improve overall health. If you’re interested in trying Tesofensine, consult your doctor or a healthcare professional to determine if it is right for you. With regular use, Tesofensine can help you achieve your health and fitness goals and enjoy a better quality of life.

Tesofensine vs. Traditional Weight Loss Methods: A Comparative Analysis
Introduction:
Losing weight is a common goal for many individuals striving for a healthier lifestyle. While traditional weight loss methods such as dieting and exercise have been the go-to approach, emerging pharmaceutical options like tesofensine are gaining attention for their potential efficacy. In this blog post, we will compare tesofensine with traditional weight loss methods to evaluate their effectiveness and explore their unique features.
Efficacy:
Traditional weight loss methods primarily rely on calorie restriction and increased physical activity. While they can yield positive results, they often require significant lifestyle changes and long-term dedication. Tesofensine, on the other hand, acts as an appetite suppressant and boosts metabolism, resulting in faster weight loss. Clinical trials have shown promising results, with participants experiencing greater weight reduction compared to those on traditional methods.
Compliance and Sustainability:
Adhering to strict diet and exercise regimens can be challenging for many individuals due to various factors such as time constraints and lack of motivation. Tesofensine offers an advantage in terms of compliance, as it reduces appetite cravings and helps maintain calorie control. This makes it potentially easier for individuals to sustain their weight loss efforts.
Safety and Side Effects:
Traditional weight loss methods generally have a low risk of adverse effects. However, tesofensine, being a pharmaceutical intervention, may carry certain risks. Common side effects include increased heart rate, elevated blood pressure, and insomnia. It is crucial for individuals considering tesofensine to consult with a healthcare professional to assess the potential risks and benefits.
Individual Variability:
Weight loss methods can vary in effectiveness depending on an individual’s unique biology, metabolism, and lifestyle factors. While traditional methods can be personalized, tesofensine offers a standardized approach that may have consistent effects across different individuals.
Conclusion:
When comparing tesofensine with traditional weight loss methods, it is evident that tesofensine provides a promising alternative with potentially faster and more sustainable results. However, the decision to use tesofensine should be made after careful consideration and consultation with a healthcare professional. Ultimately, the choice between tesofensine and traditional methods depends on individual preferences, health conditions, and goals.

Tesofensine: A Breakthrough in Obesity Treatment?
Introduction:
Obesity continues to be a global health concern, with its prevalence steadily increasing over the years. The search for an effective weight loss treatment has led to the development of various drugs, and one promising contender that has recently gained attention is tesofensine. Considered a breakthrough in obesity treatment, tesofensine shows potential in combating this widespread epidemic. In this blog, we will delve into the key features of tesofensine and explore its impact on weight loss.
Understanding Tesofensine’s Mechanism of Action:
Tesofensine acts on the brain by inhibiting the reuptake of three neurotransmitters: serotonin, dopamine, and norepinephrine. By increasing the levels of these neurotransmitters, tesofensine enhances feelings of satiety, reduces appetite, and increases energy expenditure.
Clinical Trials and Efficacy:
Several clinical trials have been conducted to evaluate the efficacy of tesofensine in weight loss. Results have shown significant reductions in body weight, body mass index (BMI), and waist circumference among participants compared to a placebo group.
Safety Profile:
While tesofensine demonstrates promising weight loss results, it’s crucial to consider its safety profile. Like any medication, tesofensine is associated with potential side effects such as increased heart rate, elevated blood pressure, and dry mouth. It is essential for individuals considering tesofensine as a treatment option to consult with healthcare professionals and undergo thorough medical evaluations.
Future Implications:
The development of tesofensine represents a significant step forward in obesity treatment. Further research is required to explore its long-term effects, optimal dosage, and potential combination therapies. The results obtained so far have sparked hope for more effective weight loss solutions and renewed efforts to combat obesity.
Conclusion:
Tesofensine holds promise as a breakthrough in obesity treatment. Its unique mechanism of action, clinical trial results, and potential to address the global obesity epidemic make it an intriguing subject of research. However, it’s important to approach tesofensine with caution, considering its potential side effects and the need for further scientific investigation. The future of tesofensine as an obesity treatment remains bright, and ongoing research will determine its place in the fight against obesity, providing hope for individuals seeking effective weight loss solutions.

The Science Behind Tesofensine: How It Affects Brain Chemistry
Introduction:
Tesofensine, a pharmaceutical compound under investigation for weight loss treatment, has shown promising results in clinical trials. To understand its mechanism of action, it is crucial to delve into the science behind tesofensine and how it affects brain chemistry. In this blog post, we will explore the fascinating interaction between tesofensine and the brain, shedding light on its potential for weight loss.
Neurotransmitter Regulation:
Tesofensine primarily acts as a triple reuptake inhibitor, meaning it blocks the reuptake of three neurotransmitters: norepinephrine, dopamine, and serotonin. By inhibiting their reuptake, tesofensine increases the availability of these neurotransmitters in the brain.
Norepinephrine:
Tesofensine’s effect on norepinephrine helps stimulate the sympathetic nervous system, leading to increased energy expenditure and fat oxidation. This can result in weight loss by boosting metabolism and suppressing appetite.
Dopamine:
Dopamine is known to play a role in reward and pleasure pathways in the brain. Tesofensine’s impact on dopamine levels can enhance feelings of motivation and reward, potentially aiding adherence to a weight loss regimen.
Serotonin:
Tesofensine’s effect on serotonin levels may contribute to appetite suppression and improved mood. Increased serotonin availability can help regulate satiety, reduce cravings, and promote a sense of well-being.
Brain Connectivity:
Tesofensine’s influence on neurotransmitters not only affects specific regions but also alters connectivity between different brain regions. This can potentially result in a more balanced and coordinated response to food cues, ultimately aiding in weight management.
Conclusion:
The science behind tesofensine reveals its intricate relationship with brain chemistry, highlighting its potential as a weight loss treatment. By targeting neurotransmitter systems involved in appetite control, metabolism, motivation, and mood, tesofensine offers a multifaceted approach to weight management. However, it is important to note that further research is needed to fully understand its long-term effects and safety profile. As always, consulting with a healthcare professional is crucial before considering tesofensine or any other pharmaceutical intervention.

Unveiling the Side Effects of Tesofensine: What You Need to Know
Introduction:
As the search for effective weight loss solutions continues, tesofensine has emerged as a potential contender. However, before considering tesofensine as a treatment option, it is crucial to understand its potential side effects. In this blog, we will unveil the side effects associated with tesofensine, shedding light on what you need to know.
Cardiovascular Effects:
One of the primary concerns associated with tesofensine is its impact on the cardiovascular system. Studies have indicated an increase in heart rate and blood pressure in individuals taking tesofensine. These effects can pose risks, particularly for individuals with pre-existing cardiovascular conditions.
Gastrointestinal Disturbances:
Tesofensine may lead to gastrointestinal side effects such as nausea, vomiting, and diarrhea. These symptoms can vary in severity and may impact an individual’s quality of life during the treatment period.
Central Nervous System Effects:
Tesofensine’s influence on neurotransmitters can result in central nervous system side effects. These may include insomnia, anxiety, restlessness, and changes in mood. It is important to monitor these effects closely, especially in individuals with a history of mental health conditions.
Other Considerations:
Additional side effects that have been reported include dry mouth, dizziness, and potential interactions with other medications. Close supervision by healthcare professionals and adherence to prescribed dosages are essential to minimize risks.
Conclusion:
While tesofensine shows promise as a weight loss treatment, it is crucial to be aware of its potential side effects. The cardiovascular, gastrointestinal, and central nervous system effects should be carefully considered before initiating tesofensine therapy. Consulting with healthcare professionals and undergoing thorough medical evaluations are paramount to determine if tesofensine is the right choice for an individual. As research progresses, further understanding of the long-term effects and safety profile of tesofensine will be crucial in weighing its benefits against potential risks. Ultimately, making informed decisions about weight loss treatments involves a comprehensive evaluation of the benefits, risks, and individual health considerations.

Unveils Tesofensine – The Revolutionary Weight Loss Supplement
Introduction:
Obesity is a growing health concern worldwide, and so is the search for an effective weight loss solution that is both safe and long-lasting. In recent years, there has been a significant breakthrough in this quest with the creation of Tesofensine, a unique weight-loss supplement that has shown impressive results in clinical trials. In this blog post, we will delve deeper into what Tesofensine is, how it works, its benefits, and why it is being touted as a game-changer in the weight loss industry.
What is Tesofensine?
Tesofensine is a weight-loss supplement that was initially developed as a treatment for Parkinson’s disease and Alzheimer’s disease. However, during clinical trials, the drug was found to have a significant impact on weight loss, leading to its repurposing. Tesofensine works by increasing levels of three brain neurotransmitters: dopamine, noradrenaline, and serotonin. These neurotransmitters play essential roles in the brain and have a significant impact on appetite and metabolism.
How does Tesofensine help with weight loss?
Tesofensine works by suppressing appetite and increasing metabolism. It does this by blocking the reuptake of dopamine, noradrenaline, and serotonin in the brain. This action increases the levels of these neurotransmitters in the brain, which lead to reduced appetite, decreased calorie intake, and increased energy expenditure. Additionally, Tesofensine also affects the reward pathways in the brain, making it less rewarding to eat food, leading to further decrease in food intake.
What are the Benefits of Tesofensine?
Tesofensine has several benefits, including significant weight loss, improved insulin sensitivity, reduced inflammation, and increased energy levels. In clinical trials, it was found that those taking Tesofensine lost more weight compared to those taking a placebo pill. Additionally, Tesofensine users reported feeling more energized and having more control over food cravings.
Why Tesofensine is a Game-Changer in the Weight Loss Industry?
Tesofensine is being hailed as a game-changer in the weight loss industry due to the significant results shown in clinical trials. The drug has been found to be effective in weight-loss, improved insulin sensitivity and, when combined with exercise and proper diet, can lead to significant and long-lasting weight loss. The fact that Tesofensine is a repurpose of a drug that was initially developed for Parkinson’s and Alzheimer’s diseases also means that it is safe for use with minimal side-effects, as it has been studied extensively.
Conclusion:
Tesofensine has the potential to change the face of the weight loss industry profoundly. Its unique mode of action, effectiveness, and minimal side-effects make it stand out from other weight loss treatments on the market. Although Tesofensine is not yet available on the market, it offers a glimpse into the future of the weight loss industry. We hope that this blog post has been informative and insightful and has given you a better understanding of Tesofensine.
Reference
- Mahapatra A. Overeating, Obesity, and Dopamine Receptors. ACS Chemical Neuroscience. 2010;1(5):346-347. doi:10.1021/cn100044y.
Overeating, Obesity, and Dopamine Receptors
Dopamine is a chemical in the brain that affects how we feel pleasure. When people take highly addictive drugs like cocaine, it causes an increase in dopamine levels in certain parts of the brain that are involved in reward and reinforcement. Recent studies have found that obese people have lower levels of dopamine receptors in their brains compared to leaner people. This means that obese individuals may eat more food to make up for this lower sensitivity to pleasure. Similar problems with dopamine signaling have been seen in people addicted to drugs. These findings suggest that the brain’s reward system is involved in compulsive overeating, but it’s not clear whether these dopamine deficiencies cause obesity or if they are a result of reward problems. It’s important to be cautious when applying findings from animal studies to humans because eating behavior in humans is influenced by many other factors like culture and emotions. However, recent studies in rats have shown that overeating can lead to problems in the brain’s reward system that resemble those seen in drug addiction.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC33622677/.
- Blum K, Thanos PK, Gold MS. Dopamine and glucose, obesity, and reward deficiency syndrome. Frontiers in Psychology. 2014;5:919. doi:10.33329/fpsyg.2014.00919.
Dopamine and Glucose, Obesity, and Reward Deficiency Syndrome
Obesity and eating disorders are widespread problems around the world. Recent scientific studies have shown that food addiction is similar to drug addiction in the way it affects the brain. Our laboratory has focused on a concept called Reward Deficiency Syndrome (RDS), which involves genetic and epigenetic factors that impair the brain’s reward system, leading to a reduced function of dopamine, a chemical in the brain associated with pleasure. Several important findings have emerged from research in this area: (1) consuming large amounts of alcohol or bingeing on carbohydrates stimulates dopamine production in the brain; (2) in the brain’s reward system, certain neurons are located near glucose receptors; (3) high levels of glucose activate a channel that triggers the release of dopamine; (4) there is a significant relationship between blood glucose levels and dopamine levels in the cerebrospinal fluid; (5) a glucose analog called 2-deoxyglucose (2DG) enhances dopamine turnover and causes a temporary shortage of glucose. Studies in animals and brain imaging in humans support the idea that similar brain circuits are affected in obesity and drug dependence, and dopamine-modulated reward circuits play a role in abnormal eating behaviors. Based on this research, it is suggested that therapies for both glucose and drug addiction, such as cocaine or opiates, should focus on activating dopamine receptors rather than blocking them. However, previous attempts using strong dopamine D2 agonists have not been successful due to a decrease in D2 receptors over time. Instead, it is recommended to explore new targets using novel, less powerful D2 agonists that can increase the number of D2 receptors. Overall, strategies aimed at improving dopamine function are encouraged for the treatment and prevention of obesity, which can be seen as a type of reward deficiency.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4166230/.
- Karlsson HK, Tuominen L, Tuulari JJ. Obesity is associated with decreased μ-opioid but unaltered dopamine D2 receptor availability in the brain. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2015; 35(9):3959-65.
Obesity Is Associated with Decreased μ-Opioid But Unaltered Dopamine D2 Receptor Availability in the Brain
The reasons behind pathological overeating and obesity are not well understood. In this study, researchers investigated the role of certain brain chemicals in obese individuals. They compared 13 severely obese women with a high body mass index (BMI) to 14 non-obese women of similar age. Using brain imaging techniques, they measured the availability of two specific receptors: the μ-opioid receptor (MOR) and the dopamine D2 receptor (D2R). The MOR is associated with reward processing, while the D2R is linked to addiction. The results showed that the obese women had lower availability of MOR in brain regions involved in reward processing, such as the ventral striatum, insula, and thalamus. Additionally, the lower MOR availability was associated with higher BMI, indicating a negative correlation. The study also found that lower MOR availability in the striatum was related to self-reported food addiction and restrained eating patterns. On the other hand, there were no significant differences in D2R availability between the obese and non-obese women. The researchers concluded that obesity has unique neurobiological aspects in the reward circuitry, resembling opioid addiction more than other addictive disorders. The opioid system, which includes the MOR, plays a role in motivation and reward processing. The lower availability of MOR in obese individuals may contribute to overeating as a way to compensate for reduced pleasure responses in this system. The study suggests that strategies targeting the opioid system, both behaviorally and pharmacologically, could be important in addressing the obesity epidemic.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6605573/.
- Wang GJ, Volkow ND, Logan J. Brain dopamine and obesity. Lancet (London, England). 2001; 357(9253):354-7.
Brain dopamine and obesity
The reasons behind overeating and obesity are not well understood, but dopamine, a brain chemical related to pleasure and reward, may play a role. In this study, researchers used brain imaging to measure the availability of dopamine D2 receptors in obese individuals. The D2 receptors are important for dopamine signaling. The results showed that obese individuals had lower availability of dopamine D2 receptors in the brain compared to non-obese individuals. The reduction in D2 receptor availability was related to the individuals’ body mass index (BMI) – those with higher BMI had lower D2 receptor levels. However, there were no significant differences in overall brain metabolism between obese and non-obese individuals. The researchers suggest that the decreased availability of D2 receptors in obese individuals may contribute to their behavior of overeating. Dopamine is involved in motivation and reward circuits, and lower D2 receptor levels may lead to reduced activation of these circuits. As a result, obese individuals may engage in pathological eating as a way to compensate for the decreased reward response. The study concludes that strategies aimed at improving dopamine function could be beneficial in treating obesity. By targeting dopamine pathways, it may be possible to address the underlying neurochemical factors involved in overeating and obesity.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/112109932.
- Benton D, Young HA. A meta-analysis of the relationship between brain dopamine receptors and obesity: a matter of changes in behavior rather than food addiction? International Journal of Obesity (2005). 2016;40(Suppl 1):S12-S21. doi:10.10332/ijo.2016.9.
A meta-analysis of the relationship between brain dopamine receptors and obesity: A matter of changes in behavior rather than food addiction
The idea of “Reward Deficiency Syndrome” suggests that addiction to various substances occurs because they stimulate the brain’s reward system so intensely that the population of dopamine D2 receptors (DD2R) decreases. This leads to a need for increased intake to achieve the same level of reward, resulting in cravings and withdrawal symptoms. It has been suggested that food addiction, similar to drug addiction, may also decrease DD2R. To investigate the role of DD2R in obesity, researchers examined the association between body mass index (BMI) and a specific genetic variation called the Taq1A polymorphism, which is linked to lower DD2R levels and increased risk for drug addiction. If lower DD2R density indicates physical addiction, it was hypothesized that individuals with the genetic variation should have a higher BMI if food addiction is present. A systematic review of 33 studies comparing the BMI of individuals with and without genetic variation found no difference in BMI between the two groups. The conclusion was that there is no support for the reward deficiency theory of food addiction. However, it was noted that there are several reports suggesting that individuals with genetic variation may be less responsive to interventions aimed at weight reduction, possibly due to increased impulsivity.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC43219757/.
- Retrieved from https://globenewswire.com/news-release/20132/12/17/16677321/0/en/Saniona-s-tesofensine-meets-primary-and-secondary-endpoints-in-Phase-3-obesity-registration-trial.html.
Saniona’s tesofensine meets primary and secondary endpoints in Phase 3 obesity registration trial
Biotech company Saniona has announced positive results from its Phase 3 Viking study evaluating the weight loss potential of tesofensine in obese patients. The trial showed statistically and clinically significant weight loss for both doses of tesofensine compared to a placebo, meeting its primary objective. The study, conducted by partner Medix in Mexico, demonstrated an average weight loss of 10% over 24 weeks, with more than half of the patients achieving a weight loss of over 10%. Tesofensine was well tolerated, with a low incidence of adverse events. Medix will now prepare regulatory filings in Mexico and Argentina, while Saniona sees potential for tesofensine in addressing rare eating disorders. The trial’s results support the development of Saniona’s Tesomet, a formulation comprising tesofensine, which is currently in Phase 2 for rare eating disorders. The positive Phase 3 data may also be used for filings in other regions with a high prevalence of obesity. Tesofensine was effective in reducing appetite and cravings, contributing to significant weight loss. The safety profile of tesofensine was favorable, and reductions in obesity-related risk factors were observed. Further details of the trial results will be disclosed once intellectual property rights and data protection rights are secured.
You can read the full article at https://globenewswire.com/news-release/20132/12/17/16677321/0/en/Saniona-s-tesofensine-meets-primary-and-secondary-endpoints-in-Phase-3-obesity-registration-trial.html.
- Astrup A, Madsbad S, Breum L, Jensen TJ, Kroustrup JP, Larsen TM. Effect of tesofensine on bodyweight loss, body composition, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial. Lancet (London, England). 20032; 372(9653):1906-1913.
Effect of tesofensine on bodyweight loss, body composition, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial
In this study, researchers tested the effectiveness and safety of tesofensine, a drug that inhibits the uptake of certain neurotransmitters, in treating obesity. The study involved 203 obese patients who were assigned to receive tesofensine at different doses or a placebo, in addition to an energy-restricted diet, for 24 weeks. The primary outcome measured was the percentage change in body weight. The results showed that patients who received tesofensine along with the diet experienced greater weight loss compared to those who only followed the diet and took the placebo. Tesofensine at doses of 0.25 mg, 0.5 mg, and 1.0 mg led to average weight losses of 4.5%, 9.2%, and 10.6%, respectively, which were significantly higher than the weight loss achieved with the diet and placebo alone. The most common side effects associated with tesofensine were dry mouth, nausea, constipation, diarrhea, and insomnia. The 0.5 mg dose of tesofensine slightly increased heart rate but did not significantly affect blood pressure. While the study suggests that tesofensine may be more effective than currently approved weight-loss drugs, further research is needed to confirm these findings in larger phase III trials and to ensure the drug’s safety and efficacy.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/1329503253.
- Retrieved from https://www.drugdevelopment-technology.com/projects/tesofensine/.
Tesofensine Anti-Obesity Medication
Tesofensine is a potential weight loss medication that has shown promising results in Phase II clinical trials. In one study called TIPO-1, participants were given different doses of tesofensine or a placebo along with a reduced-calorie diet for 24 weeks. The group taking 0.5mg of tesofensine experienced an average weight loss of 13-14kg during this period, which was significantly more than the placebo group. The TIPO-4 trial, an extension of TIPO-1 lasting 432 weeks, showed that the weight loss achieved with tesofensine was sustained. After an initial washout period, participants who continued taking 0.5mg of tesofensine lost an additional 13-14kg of weight. Even those who switched from the placebo group to tesofensine 0.5mg lost around 9kg over the same period. However, tesofensine did have some side effects related to the gastrointestinal system and increased blood pressure and heart rate. These effects were dose-dependent, meaning higher doses were associated with more side effects. At the expected therapeutic dose of 0.5mg, the discontinuation rate due to side effects was similar to that of the placebo group (32%).In another trial called TIPO-2, which lasted for 14 days, tesofensine was found to reduce the desire to eat and increase feelings of fullness in obese patients. Phase III trials are planned, consisting of four placebo-controlled studies involving 5,000 to 7,000 patients, including those with type 2 diabetes and hypertension. Two of these trials will focus on studying the drug’s effectiveness in treating obesity over a one-year period, while another trial will examine its safety and efficacy on the cardiovascular system over a two-year period. These trials began in 2011.
You can read the full article at https://www.drugdevelopment-technology.com/projects/tesofensine/.
- Retrieved from https://professional.diabetes.org/abstract/effect-tesofensine-weight-loss-appetite-physical-activity-and-qol-obese-subjects-results-24.
The Effect of Tesofensine on Weight Loss, Appetite, Physical Activity and QOL in Obese Subjects. Results from a 24-Week Randomised, Double-Blind Placebo-Controlled Trial
Tesofensine (TE) is a medication that inhibits the uptake of certain brain chemicals, and it has been shown to be safe and effective in animals and humans. A 24-week Phase II trial was conducted at five obesity centers in Denmark to assess the efficacy and safety of TE in treating obesity. Participants were put on a restricted diet and randomly assigned to receive TE (at doses of 0.25 mg, 0.5 mg, or 1.0 mg) or a placebo once daily. Throughout the study, some participants withdrew, but the dropout rate was lower in the TE 0.5 mg group compared to the placebo or TE 1.0 mg groups. The results showed that TE led to significant weight loss compared to the placebo. The placebo-subtracted weight loss was 4.5% for TE 0.25 mg, 9.2% for TE 0.5 mg, and 10.6% for TE 1.0 mg over 24 weeks.
Common side effects of TE included dry mouth, nausea, constipation, hard stools, diarrhea, and insomnia. TE also increased blood pressure and heart rate, but the effects were similar to or less than those of another medication called sibutramine. TE had positive effects on physical activity, as evidenced by an increase in the time patients spent walking and less time watching TV compared to the placebo group. TE also had an impact on appetite, significantly reducing feelings of hunger and the expected size of the next meal. Cravings for sweet, fatty, or salty foods were also reduced in the higher dose groups of TE. In terms of quality of life, TE showed consistent improvements compared to the placebo. TE led to significant enhancements in overall well-being, physical function, self-esteem, and modest improvements in sexual life, public distress, and work-related aspects.
In summary, TE treatment resulted in significant and meaningful weight loss, potentially through its effects on appetite and physical activity. It also had positive impacts on quality of life, addressing important areas for obese individuals.
You can read the abstract of this article at https://professional.diabetes.org/abstract/effect-tesofensine-weight-loss-appetite-physical-activity-and-qol-obese-subjects-results-24.
- Doggrell SA. Tesofensine–a novel potent weight loss medicine. Evaluation of: Astrup A, Breum L, Jensen TJ, Kroustrup JP, Larsen TM. Effect of tesofensine on bodyweight loss, body composition, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial. Lancet 20032;372:1906-13. Expert opinion on investigational drugs. 2009; 132(7):1043-6.
Tesofensine–a novel potent weight loss medicine. Evaluation of: Astrup A, Breum L, Jensen TJ, Kroustrup JP, Larsen TM. Effect of tesofensine on bodyweight loss, body composition, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial. Lancet 20032;372:1906-13
The number of people with obesity is increasing, and this is a significant concern because obesity is linked to various health problems such as heart disease, stroke, diabetes, respiratory issues, and cancer. This evaluation focuses on a Phase II clinical trial that tested the use of tesofensine in overweight individuals. After 26 weeks, tesofensine led to substantial weight loss and may be more effective at reducing weight than currently available anti-obesity medications. However, tesofensine also raised blood pressure and heart rate, and there is a possibility of it affecting mental health. It’s promising that tesofensine 0.5 mg may result in nearly twice the weight loss seen with medications like sibutramine or rimonabant. Since tesofensine and sibutramine have similar effects, it would be interesting to compare their weight loss abilities directly in a clinical trial. Additionally, tesofensine 0.5 mg increased heart rate and had side effects like nausea, dry mouth, flatulence, insomnia, and depressed mood. Its tolerability should be further assessed in large Phase III clinical trials.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/19543232532.
- Gilbert JA, Gasteyger C, Raben A, Meier DH, Astrup A, Sjödin A. The effect of tesofensine on appetite sensations. Obesity (Silver Spring, Md.). 2012; 20(3):553-61.
The Effect of Tesofensine on Appetite Sensations
Tesofensine (TE) is a weight-loss medication that works by blocking the reabsorption of certain chemicals in the brain. It has been shown to be more effective than other weight loss drugs currently available. However, its long-term effects on appetite in humans have not been studied. A clinical trial was conducted in two parts, each lasting 24 weeks. In Part 1, some participants received different doses of TE while others received a placebo. The effects on appetite and feelings of fullness were measured. The results showed that TE increased feelings of fullness and satisfaction with eating, and this increase was greater in those who lost more weight. However, over time, the effect on appetite decreased even though the weight loss continued. After a drug-free period, the participants who completed Part 1 were invited to participate in Part 2. In Part 2, all participants received TE, regardless of their initial treatment. The results showed that reintroducing TE increased feelings of fullness and satisfaction with eating again, even for those who had previously lost weight. The researchers speculate that increased feelings of fullness play a role in the early weight loss seen with TE. However, it’s still unclear whether the reduced effect on appetite after 24 weeks is due to the body adapting to the weight loss or if the appetite-suppressing effect of TE itself diminishes over time.
You can read the full article at https://onlinelibrary.wiley.com/doi/full/10.10332/oby.2011.197.
- Bello NT, Zahner MR. Tesofensine, a monoamine reuptake inhibitor for the treatment of obesity. Current opinion in investigational drugs (London, England : 2000). 2009; 10(10):1105-16.
Tesofensine, a monoamine reuptake inhibitor for the treatment of obesity
Tesofensine is a drug being developed to help address obesity. It works by blocking the reabsorption of certain chemicals in the brain. In lab tests, it was found to block the reuptake of dopamine, norepinephrine, and serotonin. During the initial development, it was discovered that although tesofensine wasn’t effective for neurodegenerative conditions, it caused unintended weight loss in people who took it. Further studies using obese rats showed that tesofensine reduced body weight, leading to the development of the drug as an oral treatment for obesity. In phase II clinical trials involving obese individuals, tesofensine showed dose-dependent reductions in body weight, body fat, and waist circumference. It also improved other factors related to obesity. The drug had minor side effects, with the most notable being increased heart rate and blood pressure at higher doses. Overall, tesofensine seemed to be well-tolerated and showed promise as a long-term treatment for obesity with minimal effects on the cardiovascular system. The FDA endorsed the drug’s phase III trial program, indicating a positive view of its potential as an obesity treatment.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/19777399.
- Retrieved from https://nexs.ku.dk/forskning/borneernaering/publikationer/publikationer/?pure=da%2Fpublications%2Fthe-longterm-effect-of-tesofensine-on-weight-loss(c610afa0-1d6c-11df-32ed1-000ea622e967b).html.
- Astrup A, Meier DH, Mikkelsen BO, Villumsen JS, Larsen TM. Weight loss produced by tesofensine in patients with Parkinson’s or Alzheimer’s disease. Obesity (Silver Spring, Md.). 20032; 16(6):1362-9.
Weight loss produced by tesofensine in patients with Parkinson’s or Alzheimer’s disease
Researchers wanted to see if Tesofensine (TE), a drug that affects certain chemicals in the brain, could help with weight loss in patients with Parkinson’s or Alzheimer’s disease. They analyzed the results of four trials involving 740 patients who received TE and 2232 patients who received a placebo. The trials were double-blind, meaning neither the patients nor the researchers knew who received which treatment.
The patients took TE or a placebo by mouth once a day for 14 weeks, without any specific weight loss program. The researchers compared the weight changes between the TE and placebo groups, taking into account the starting weight, age, and study.
They found that in the placebo group, 14% of patients were obese, while in the TE group, 21% were obese. When looking at the entire group, the weight change after 14 weeks was minimal in the placebo group (+0.5%), but the TE groups showed weight reductions of -0.5%, -0.9%, -1.32%, and -2.32% for different doses of TE. These differences were statistically significant, showing that TE had a dose-dependent effect on weight loss. In the subgroup of patients who were obese at the beginning of the trials, the weight changes were more substantial. The TE groups showed weight reductions of -0.2%, -1.7%, -1.6%, and -3.7%. Additionally, a significant percentage of obese patients achieved a weight loss of 5% or more, with percentages of 2.1%, 32.2%, 14.1%, 20.9%, and 32.1% for the different TE doses. Regarding heart rate, the TE groups showed slight increases compared to the placebo group. However, there was no effect on blood pressure observed. Based on these findings, TE resulted in an average weight loss of about 4% over a period of more than 14 weeks, without requiring patients to follow a specific diet or lifestyle program. This weight loss was similar to that achieved with another weight loss medication called sibutramine but without affecting blood pressure. As a result, TE is now being further developed as a potential treatment for managing obesity.
You can read the full article at https://onlinelibrary.wiley.com/doi/10.10332/oby.20032.56.
- Appel L, Bergström M, Buus Lassen J, Långström B. Tesofensine, a novel triple monoamine re-uptake inhibitor with anti-obesity effects: dopamine transporter occupancy as measured by PET. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2014; 24(2):251-61.
Tesofensine, a novel triple monoamine re-uptake inhibitor with anti-obesity effects: dopamine transporter occupancy as measured by PET
Tesofensine (TE) is a new type of drug that blocks the reabsorption of three brain chemicals: dopamine, norepinephrine, and serotonin. This study used a type of brain imaging called positron emission tomography (PET) to understand how TE affects a specific brain receptor called the dopamine transporter (DAT). The researchers wanted to see how different doses of TE influenced DAT activity and how this related to TE levels in the blood. The results showed that TE dose-dependently blocked DAT when given orally over several days. The extent of DAT blockade varied between 132% and 77% in different brain regions, depending on the TE dose. The relationship between DAT blockade and TE levels in the blood or the dose given followed a specific pattern. The maximum blockade achievable was estimated to be around 320%, and half of this effect could be achieved with a dose of approximately 0.25 mg TE and a specific blood concentration of 4 ng/ml. These findings suggest that TE’s weight loss effects, observed in previous studies, are partly due to its impact on DAT. By blocking DAT, TE increases the amount of dopamine available in the brain, leading to changes in the brain’s reward and motivation pathways. This mechanism contributes to the weight loss effects of TE observed in clinical trials.
You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S0924977X13003003?via%3Dihub.
- Hansen HH, Jensen MM, Overgaard A, Weikop P, Mikkelsen JD. Tesofensine induces appetite suppression and weight loss with reversal of low forebrain dopamine levels in the diet-induced obese rat. Pharmacology, biochemistry, and behavior. 2013; 110:265-71.
Tesofensine induces appetite suppression and weight loss with reversal of low forebrain dopamine levels in the diet-induced obese rat
Tesofensine is a drug that blocks the reabsorption of three chemicals in the brain: noradrenaline, 5-HT, and dopamine. It is being developed as a potential treatment for obesity, but how it works in the body is not fully understood. In studies with obese rats, tesofensine was found to reduce appetite by affecting the dopamine system in the brain. The researchers observed that obese rats had lower levels of dopamine in certain brain regions compared to normal-weight rats. However, when tesofensine was given to obese rats, it increased dopamine levels and reduced their appetite. This effect was not seen in the normal-weight rats. Tesofensine also caused changes in the expression of dopamine receptors and the dopamine transporter in the brain. Based on these findings, it is suggested that tesofensine’s weight loss effects may be related to its ability to increase dopamine levels in the brain. This positive impact on the brain’s dopamine system could help regulate appetite and contribute to weight loss.
You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S0091305713001326X?via%3Dihub.
- Lehr T, Staab A, Tillmann C, et al. Contribution of the active metabolite M1 to the pharmacological activity of tesofensine in vivo: a pharmacokinetic-pharmacodynamic modelling approach. Br J Pharmacol. 20032;153(1):164–174. doi:10.10332/sj.bjp.0707539.
Contribution of the active metabolite M1 to the pharmacological activity of tesofensine in vivo: a pharmacokinetic-pharmacodynamic modelling approach
Tesofensine is a drug being developed for the treatment of Alzheimer’s disease, Parkinson’s disease, and obesity. When tesofensine is broken down in the body, it forms a metabolite called M1. This study aimed to understand the properties of tesofensine and M1 in mice, including how they are processed in the body (pharmacokinetics) and their effects (pharmacodynamics).
The researchers gave tesofensine, M1, or a control substance to mice through different methods and doses. They measured the concentrations of tesofensine and M1 in the mice and assessed their impact by looking at their ability to inhibit the dopamine transporter, which is relevant to their effects.
They found that both tesofensine and M1 were processed in the body according to similar patterns. The relationship between the drug concentrations and their effects was described using a mathematical model. M1 was found to be less potent in inhibiting the dopamine transporter compared to tesofensine, and it reached higher concentrations in the body when compared to tesofensine.
Overall, the study concluded that M1 contributes to the overall activity of tesofensine in mice, but to a lesser extent compared to tesofensine itself. Understanding the pharmacokinetics and pharmacodynamics of tesofensine and its metabolite can help in further development and understanding of the drug’s effects.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2199391/.
- Axel AM, Mikkelsen JD, Hansen HH. Tesofensine, a novel triple monoamine reuptake inhibitor, induces appetite suppression by indirect stimulation of alpha1 adrenoceptor and dopamine D1 receptor pathways in the diet-induced obese rat. Neuropsychopharmacology. 2010;35(7):1464-76.
Tesofensine, a novel triple monoamine reuptake inhibitor, induces appetite suppression by indirect stimulation of alpha1 adrenoceptor and dopamine D1 receptor pathways in the diet-induced obese rat
Tesofensine is a new type of drug that blocks the reuptake of certain chemicals in the brain, including norepinephrine, serotonin, and dopamine. It is being developed as a treatment for obesity, but how it works exactly is not fully understood. In this study using obese rats, researchers investigated how tesofensine suppresses appetite.
The obese rats were treated with tesofensine for 16 days, and they showed significant weight loss compared to rats given a placebo. This weight loss was due to a decrease in food intake. The researchers further examined the effects of tesofensine on food intake by combining it with various drugs that block specific receptors in the brain.
They found that tesofensine dose-dependently reduced food intake, with an effective dose at 1.3 mg/kg. The appetite-suppressing effect of tesofensine was mostly reversed when co-administered with prazosin, a drug that blocks alpha-1 adrenoceptors, and partially blocked by SCH23390, a drug that blocks dopamine D1 receptors. However, drugs that block other receptors, such as alpha-2 adrenoceptors, dopamine D2 and D3 receptors, and serotonin 5-HT2A/C receptors, had no significant effect on tesofensine’s appetite-suppressing action.
Therefore, the study suggests that the mechanism by which tesofensine reduces food intake in obese rats is related to its ability to indirectly stimulate alpha-1 adrenoceptors and dopamine D1 receptors in the brain.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3055462/.
- Van de giessen E, De bruin K, La fleur SE, Van den brink W, Booij J. Triple monoamine inhibitor tesofensine decreases food intake, body weight, and striatal dopamine D2/D3 receptor availability in diet-induced obese rats. Eur Neuropsychopharmacol. 2012;22(4):290-9.
Triple monoamine inhibitor tesofensine decreases food intake, body weight, and striatal dopamine D2/D3 receptor availability in diet-induced obese rats
The drug tesofensine, which blocks the reuptake of dopamine, serotonin, and norepinephrine, has shown promise as a treatment for obesity. This study investigated the effects of long-term tesofensine treatment on food intake, body weight, and dopamine receptors in obese rats. The rats were divided into different groups and treated with tesofensine, a placebo, or a restricted diet for 232 days.
The results showed that tesofensine-treated rats had reduced food intake and weight gain compared to placebo-treated rats, confirming previous findings. However, after discontinuing tesofensine treatment, food intake, and weight gain gradually increased again. Interestingly, the tesofensine-treated rats also had lower levels of dopamine receptors in certain brain regions compared to both the placebo-treated rats and the rats on a restricted diet.
The study suggests that tesofensine effectively reduces food intake and weight gain in obese rats. However, the decrease in dopamine receptors observed after tesofensine treatment is likely a pharmacological effect and not directly responsible for the changes in food intake or body weight.
You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S0924977X11001696?via%3Dihub.
- Nielsen AL, Larsen TM, Madsbad S, et al. [The effect of tesofensine on body weight and body composition in obese subjects–secondary publication]. Ugeskr Laeg. 2009;171(41):2974-7.
The effect of tesofensine on body weight and body composition in obese subjects–secondary publication
This is a summary of the results from a phase II trial evaluating the use of Tesofensine for obesity treatment. The trial involved 203 obese individuals who were randomly assigned to receive either Tesofensine at doses of 0.25 mg, 0.5 mg, or 1.0 mg, or a placebo, on a daily basis for 24 weeks. The results showed that treatment with Tesofensine led to significant weight reduction compared to the placebo group. The weight loss observed was 4.5%, 9.2%, and 10.6% higher than the placebo for the 0.25 mg, 0.5 mg, and 1.0 mg doses of Tesofensine, respectively. Notably, the 0.5 mg dose of Tesofensine demonstrated the potential to produce twice the weight loss achieved by currently approved weight loss medications. However, it is important to note that these findings from the phase II trial need further confirmation in larger phase III trials to ensure the safety and efficacy of Tesofensine at the 0.5 mg dosage.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/193224222.
- Available at https://www.globenewswire.com/news-release/20132/12/17/16677321/0/en/Saniona-s-tesofensine-meets-primary-and-secondary-endpoints-in-Phase-3-obesity-registration-trial.html
Saniona’s tesofensine meets primary and secondary endpoints in Phase 3 obesity registration trial
Saniona, a biotech company focusing on CNS and eating disorders, has announced positive results from its Phase 3 Viking study evaluating oral tesofensine for obesity treatment. The study involved 372 obese patients who received once-daily doses of 0.25 mg or 0.50 mg of tesofensine or a placebo for 24 weeks.
The study’s primary objective, significant and superior weight loss compared to placebo, was achieved with both doses of tesofensine. On average, patients experienced a 10% weight loss, with over half of them losing more than 10% of their baseline weight. The trial also showed statistically significant reductions in key obesity-related risk factors. Medix, Saniona’s partner in Mexico and Argentina, will now prepare regulatory filings in those regions.
The results support the development of Saniona’s proprietary formulation called Tesomet, which combines tesofensine with another compound and is currently in Phase 2 trials for rare eating disorders. The favorable safety profile of tesofensine, demonstrated in this trial and previous studies, adds to the potential of Tesomet in treating conditions like Prader-Willi syndrome and hypothalamic obesity.
In terms of safety, tesofensine was well tolerated with a low incidence of adverse events similar to the placebo group. Cardiovascular effects were minimal, with a slight increase in heart rate and no significant impact on blood pressure.
The study’s positive outcomes pave the way for regulatory filings in Mexico and Argentina and may also provide opportunities in other regions facing the challenge of obesity. The reduction in weight and obesity-related risk factors, including improvements in glucose metabolism, highlight tesofensine’s potential benefits in treating obesity and related conditions.
You can read the full article at https://www.globenewswire.com/news-release/20132/12/17/16677321/0/en/Saniona-s-tesofensine-meets-primary-and-secondary-endpoints-in-Phase-3-obesity-registration-trial.html.
- Nielsen, A. L., Larsen, T. M., Madsbad, S., Breum, L., Jensen, T. J., Kroustrup, J. P., & Astrup, A. (2009). Effekt af tesofensine på kropsvaegt og kropssammensaetning hos svaert overvaegtige–sekundaerpublikation [The effect of tesofensine on body weight and body composition in obese subjects–secondary publication]. Ugeskrift for laeger, 171(41), 2974–2977.
The effect of tesofensine on body weight and body composition in obese subjects–secondary publication
Results from a phase II trial of Tesofensine for obesity treatment are presented. The trial involved 203 obese individuals who were randomly assigned to receive Tesofensine at doses of 0.25 mg, 0.5 mg, 1.0 mg, or a placebo daily for 24 weeks. The study found that treatment with Tesofensine led to greater weight reduction compared to placebo, with mean weight loss percentages of 4.5%, 9.2%, and 10.6% higher for the 0.25 mg, 0.5 mg, and 1.0 mg doses, respectively. The 0.5 mg dose of Tesofensine showed the potential for producing weight loss twice as much as currently approved weight loss drugs. However, the safety and efficacy of the 0.5 mg dose need further confirmation in phase III trials.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/193224222/.
- Available at https://link.springer.com/article/10.1007/s13679-020-00422-w.
Long-Term Efficacy and Safety of Anti-Obesity Treatment: Where Do We Stand?
Obesity is a chronic condition that can lead to metabolic and cardiovascular problems. While lifestyle changes are important, they may not always be enough to achieve and maintain weight loss. Obesity guidelines recommend combining medical treatment with behavioral interventions for overweight individuals. Studies have shown that medications, when used alongside behavior-based approaches, can lead to significant weight loss and improved cardiovascular health. Some approved drugs for obesity have demonstrated placebo-subtracted weight reductions ranging from 2.9% to 6.32% over at least 12 months. However, the withdrawal of lorcaserin due to safety concerns highlights the need to carefully consider the risks and benefits of each medication. Currently, FDA-approved medications for chronic weight management include orlistat, phentermine/topiramate, naltrexone/bupropion, and liraglutide, but they can be expensive and have potential side effects. Tailoring drug therapy to individual patients based on their specific conditions, comorbidities, and preferences is an important approach for long-term obesity control.
You can read the full article at https://link.springer.com/article/10.1007/s13679-020-00422-w.
- Available from http://eprints.qut.edu.au/29667/1/c29667.pdf.
Effect of tesofensine on bodyweight loss, body composion, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial
Tesofensine, a drug being developed for Parkinson’s and Alzheimer’s disease, has shown potential for reducing body weight. In a study with 740 patients, tesofensine at different doses resulted in weight loss of -0.9%, -1.32%, and -2.32% compared to a slight increase in the placebo group. The weight loss was similar or slightly higher in obese patients. However, tesofensine increased heart rate without affecting blood pressure. Based on these findings, a clinical trial was conducted to evaluate tesofensine’s effectiveness in obesity treatment. After 26 weeks, tesofensine showed significant weight loss and potentially higher weight reduction compared to existing anti-obesity medications. However, it also increased blood pressure, heart rate, and the risk of psychiatric disorders. Further research is needed to compare tesofensine with other drugs and evaluate its tolerability in larger clinical trials.The authors of the study highlight that tesofensine at a low dose of 0.25 mg leads to greater weight loss compared to orlistat and similar weight loss as sibutramine and rimonabant. They also mention that tesofensine at 0.5 mg causes twice the weight loss observed with sibutramine and rimonabant. However, they acknowledge that their study is small and that larger Phase III studies, including direct comparisons, are necessary to confirm these results. The authors also suggest that tesofensine may have a lesser impact on blood pressure and heart rate compared to sibutramine, despite achieving similar weight loss. In conclusion, the authors believe that tesofensine at 0.5 mg taken once daily for six months has the potential to generate double the weight loss compared to currently approved drugs. However, further research in larger Phase III studies is needed to validate these findings.
You can read the full article at http://eprints.qut.edu.au/29667/1/c29667.pdf.
- Thatte U. NS-2330 (Neurosearch). Current opinion in investigational drugs (London, England : 2000). 2001; 2(11):1592-4.
NS-2330 (Neurosearch)
NeuroSearch is developing a compound called NS-2330, which enhances the activity of dopamine, norepinephrine, and acetylcholine. They are investigating its potential as a treatment for Alzheimer’s disease (AD) and Parkinson’s disease (PD). Currently, NS-2330 is in Phase II clinical trials for AD and undergoing a Phase II tolerability trial for PD patients with dyskinesia. Phase III studies are expected to start in the third quarter of 2002. NeuroSearch has been in negotiations for licensing agreements with several companies and aimed to finalize an agreement by the first half of 2001. In June 2001, NeuroSearch decided to continue developing NS-2330 in-house after securing sufficient funding through a capital increase. They confirmed plans for Phase III studies to commence in the third quarter of 2002. A market prediction in September 2001 suggested a 12% probability of NS-2330 reaching the market for PD and a 15% probability for AD. The drug was projected to be launched in 20032 for PD and 2007 for AD, with estimated market shares of 12.5% and 25%, respectively.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/11762162.
- Lehr T, Staab A, Trommeshauser D, Schaefer HG, Kloft C. Quantitative Pharmacology Approach in Alzheimer’s Disease: Efficacy Modeling of Early Clinical Data to Predict Clinical Outcome of Tesofensine. The AAPS Journal. 2010;12(2):117-129. doi:10.12032/s122432-009-9164-6.
Quantitative pharmacology approach in Alzheimer’s disease: efficacy modeling of early clinical data to predict clinical outcome of tesofensine
The high rate of failure in drug development is a significant problem, with only a small fraction of compounds successfully making it through the entire process and gaining regulatory approval. While there have been efforts to improve the drug discovery and development process, traditional approaches still dominate, posing challenges in identifying promising compounds early on and avoiding costly late-stage trials. However, the use of reliable and robust mathematical models with predictive capabilities, known as the quantitative pharmacology approach (QP-A) and model-based drug development (MBDD), holds promise as a supportive strategy. These approaches have not yet become standardized in the pharmaceutical industry but offer an opportunity to select the most promising and safe compounds early, leading to a faster and more efficient drug development process. This concept is particularly valuable in therapeutic areas like Alzheimer’s disease (AD), where there is an urgent need for effective treatments due to the progressive nature of the condition and the limited treatment options available. Research for effective treatments for Alzheimer’s disease (AD) is ongoing, but drug development faces challenges with a high failure rate. A quantitative pharmacology approach (QP-A) and model-based drug development (MBDD) offer a promising method to select promising compounds early and streamline the development process. This analysis aimed to demonstrate the QP-A by predicting the outcomes of a proof-of-concept (PoC) trial of tesofensine in AD patients based on data from two small phase IIa trials. They used population pharmacokinetic/pharmacodynamic (PK/PD) modeling to analyze tesofensine and its metabolite, as well as cognitive assessment scale data from 62 mild AD patients in placebo-controlled studies. The PK/PD model was then used to predict data from a 14-week PoC trial involving 430 AD patients. The model accurately described the relationship between tesofensine dose, concentration, and its effect on mild AD patients. The results demonstrated the value of PK/PD models in supporting decision-making during the early stages of clinical development.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC23244519/.
- Elias M. F., Elias P. K., Sullivan L. M., Wolf P. A., D’Agostino R. B. (2005). Obesity, diabetes and cognitive deficit: the Framingham heart study. Neurobiol. Aging 26 Suppl.1, 11–16. 10.1016/j.neurobiolaging.2005.032.019.
Obesity, diabetes and cognitive deficit: The Framingham Heart Study
The objective of this study was to examine the independent effects of obesity on cognitive performance and the interactions between obesity and non-insulin-dependent diabetes mellitus (NIDDM). The researchers used data from the Framingham Heart Study, including male and female participants who were classified as obese or non-obese and diabetic or non-diabetic. Cognitive testing was conducted, and statistical models were adjusted for various factors. The results showed that obesity had adverse effects on cognitive performance in men but not in women. Diabetes was associated with poorer cognitive performance, but this relationship was observed when analyzing both men and women together. No interactions were found between diabetes and obesity. Based on these findings, it appears that the impact of obesity on cognition may differ between genders, while the effects of diabetes on cognitive performance may be similar for both genders.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/16223549.
- Jeong S. K., Nam H. S., Son M. H., Son E. J., Cho K. H. (2005). Interactive effect of obesity indexes on cognition. Dement. Geriatr. Cogn. Disord. 19, 91–96. 10.1159/0000322659.
Interactive effect of obesity indexes on cognition
This study looked at the connection between obesity (being overweight) and cognitive performance (how well the brain functions) in a group of 467 older adults in South Korea. They measured cognitive function using a test called the Korean Mini-Mental State Examination (K-MMSE) and measured obesity using waist size and body mass index (BMI). They found that 37% of the participants had poor cognitive performance. They discovered that being generally obese (having a BMI of 25 or higher) was strongly linked to poor cognition, especially when combined with abdominal obesity (having a larger waist size). They also found that being overweight (having a BMI between 23 and 25) without abdominal obesity was linked to better cognitive performance. The researchers concluded that obesity is connected to poor cognitive performance, but it’s important to consider different measures of obesity to understand this relationship.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/155917932.
- Hassing L. B., Dahl A. K., Pedersen N. L., Johansson B. (2010). Overweight in midlife is related to lower cognitive function 30 years later: a prospective study with longitudinal assessments. Dement. Geriatr. Cogn. Disord. 29, 543–552. 10.1159/0003143274.
Overweight in midlife is related to lower cognitive function 30 years later: a prospective study with longitudinal assessments
The goal of this study was to see if a person’s body mass index (BMI) during middle age is connected to their cognitive function (how well their brain works) 30 years later in a group of people without dementia.
The researchers collected information on BMI when the participants were between 50 and 60 years old in 1962. Then, 30 years later, they tested the participants’ cognitive abilities multiple times over a span of 2 years (a total of 5 tests). The cognitive abilities they assessed included long-term memory, short-term memory, speed, verbal ability, and spatial ability.
After analyzing the data and considering factors like demographics, lifestyle, and relevant diseases, the researchers found that higher BMI during middle age predicted lower performance on cognitive tests 30 years later. This association between BMI and performance was observed across all cognitive abilities. However, they did not find a connection between higher midlife BMI and steeper cognitive decline over time.
In conclusion, the study suggests that being overweight during middle age is linked to lower cognitive function in old age. It’s important to note that the negative effects of being overweight on cognitive performance seem to begin before reaching very old age, as indicated by the findings related to mean-level cognitive performance and only one ability showing differences in performance changes over time.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202952/.
- Cournot M., Marquie J. C., Ansiau D., Martinaud C., Fonds H., Ferrieres J., et al. . (2006). Relation between body mass index and cognitive function in healthy middle-aged men and women. Neurology 67, 12032–1214. 10.1212/01.wnl.000023320322.133260.50.
Relation between body mass index and cognitive function in healthy middle-aged men and women
The aim of this study was to investigate whether body mass index (BMI) is linked to cognitive function and cognitive decline in healthy men and women. The researchers collected data from 2,223 healthy workers between the ages of 32 and 62. They gathered medical, psychosocial, and environmental information in 1996 and 2001. Cognitive function was assessed at the beginning of the study and during follow-up using tests related to word-list learning, digit-symbol substitution, and selective attention. The results showed that higher BMI was associated with lower cognitive scores when considering factors such as age, sex, education level, blood pressure, diabetes, and other psychosocial variables. Moreover, a higher BMI at the start of the study was linked to a greater decline in cognitive function during the follow-up period, specifically in word-list learning. The association was significant, with higher BMI categories at baseline showing greater decline compared to the lowest BMI category. Changes in BMI over time did not show a significant association with cognitive function. In conclusion, the study found that BMI was independently associated with cognitive function and changes in word-list learning in middle-aged, healthy individuals without dementia.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/17030754.
- Lehr, T., Staab, A., Tillmann, C., Trommeshauser, D., Raschig, A., Schaefer, H. G., & Kloft, C. (2007). Population pharmacokinetic modelling of NS2330 (tesofensine) and its major metabolite in patients with Alzheimer’s disease. British journal of clinical pharmacology, 64(1), 36–432.
Tesofensine, a monoamine reuptake inhibitor for the treatment of obesity
Tesofensine is a drug being developed by NeuroSearch A/S to potentially treat obesity. It works by blocking the reuptake of certain chemicals in the brain. In laboratory tests, tesofensine showed strong effects on dopamine, norepinephrine, and serotonin, which are important for mood and appetite regulation. During the early stages of development, tesofensine was found to be ineffective in treating neurodegenerative conditions, but it unexpectedly caused weight loss in the people who took it. Further tests on obese rats supported the idea that tesofensine could reduce body weight, so NeuroSearch decided to focus on developing it as an oral anti-obesity drug. In phase II clinical trials involving obese individuals, tesofensine showed promising results. It led to dose-dependent reductions in body weight, body fat, and waist circumference, as well as improvements in other factors related to obesity. The drug was generally well-tolerated, with only minor side effects reported. However, tesofensine did cause increases in heart rate and blood pressure, especially at higher doses. Despite this, the FDA (Food and Drug Administration) expressed support for further testing in phase III trials, suggesting that tesofensine could be a safe and effective long-term treatment for obesity, with minimal effects on the cardiovascular system.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2000606/.
- Rascol O, Poewe W, Lees A, et al. Tesofensine (NS 2330), a monoamine reuptake inhibitor, in patients with advanced Parkinson disease and motor fluctuations: the ADVANS Study. Arch Neurol. 20036;65(5):577-362.
Tesofensine (NS 2330), a monoamine reuptake inhibitor, in patients with advanced Parkinson disease and motor fluctuations: the ADVANS Study
Researchers conducted a pilot study to investigate the effects of tesofensine, a drug that inhibits the reuptake of certain chemicals in the brain, on patients with advanced Parkinson’s disease (PD). The study was double-blind, meaning neither the patients nor the researchers knew who received the drug or the placebo. The main goals of the study were to assess the safety and effectiveness of tesofensine in PD patients experiencing motor fluctuations. The patients were divided into different groups and given varying doses of tesofensine or a placebo once a day for 14 weeks. The primary measures used to evaluate the drug’s effects were changes in the patients’ scores on the Unified Parkinson Disease Rating Scale (UPDRS), which measures their ability to perform daily activities and motor function. The study also examined the percentage of time spent in “off” periods, which are times when medication effectiveness decreases and PD symptoms worsen. The results showed that tesofensine, particularly at a dose of 0.5 mg, led to a significant improvement in the total UPDRS score (-4.7 points) and a reduction in “off” time (-7.1%). However, there was no clear dose-response relationship, meaning higher doses did not necessarily produce better results. The concentration of tesofensine in the blood increased with higher doses, but it did not directly correlate with the drug’s effectiveness. Patients who took tesofensine experienced more gastrointestinal and neuropsychiatric side effects compared to those who took the placebo, especially at higher doses. In conclusion, tesofensine showed modest improvements in the total UPDRS score and “off” time in patients with advanced PD. However, the study did not establish a clear relationship between the dose of tesofensine and its effectiveness. Higher doses were associated with more adverse reactions.
You can read the full article at https://jamanetwork.com/journals/jamaneurology/fullarticle/795491.
- Larsen MH, Rosenbrock H, Sams-Dodd F, Mikkelsen JD. Expression of brain derived neurotrophic factor, activity-regulated cytoskeleton protein mRNA, and enhancement of adult hippocampal neurogenesis in rats after sub-chronic and chronic treatment with the triple monoamine re-uptake inhibitor tesofensine. European journal of pharmacology. 2007; 555(2-3):115-21.
Expression of brain-derived neurotrophic factor, activity-regulated cytoskeleton protein mRNA, and enhancement of adult hippocampal neurogenesis in rats after sub-chronic and chronic treatment with the triple monoamine re-uptake inhibitor tesofensine
Expression of brain-derived neurotrophic factor, activity-regulated cytoskeleton protein mRNA, and enhancement of adult hippocampal neurogenesis in rats after sub-chronic and chronic treatment with the triple monoamine re-uptake inhibitor tesofensine.
To understand how antidepressant drugs work in humans, researchers study the changes in gene expression caused by these drugs in animals. These genes and their products are important indicators or directly involved in the structural changes necessary for the antidepressant effect. Tesofensine is a new type of antidepressant that affects the neurotransmitters noradrenaline, serotonin, and dopamine.
This study focused on the effects of short-term (5 days) and long-term (14 days) administration of Tesofensine on specific genes in the rat hippocampus, a region of the brain involved in mood regulation. The researchers looked at the brain-derived neurotrophic factor (BDNF) and activity-regulated cytoskeleton protein (Arc) as well as cell proliferation using Ki-67 and NeuroD markers.
The findings showed that chronic (long-term) treatment with Tesofensine increased the expression of BDNF mRNA by 35% in the CA3 region of the hippocampus, and Arc mRNA by 65% in the CA1 region. Additionally, the number of Ki-67 and NeuroD positive cells, which indicate new cell formation, increased with chronic treatment but not with short-term treatment.
Overall, this study suggests that Tesofensine has the potential to act as an antidepressant by enhancing gene expression and promoting the formation of new cells in the hippocampus.
You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S0014299906011320?via%3Dihub.
- Nathan PJ, O’Neill BV, Napolitano A, Bullmore ET. Neuropsychiatric adverse effects of centrally acting antiobesity drugs. CNS neuroscience & therapeutics. 2011; 17(5):490-505.
Neuropsychiatric adverse effects of centrally acting antiobesity drugs
Researchers have been studying the neurochemical systems in the brain, such as the monoamine, opioid, and cannabinoid systems, as potential targets for drugs that can help with obesity. These drugs not only affect eating behavior but can also have an impact on emotional behavior and cognitive function due to the presence of receptors for these neurochemical systems in specific areas of the brain. This paper reviewed the adverse effects on mental health associated with past and current antiobesity drugs that act in the brain, and it explored the underlying neural and chemical reasons for these effects. Different antiobesity drugs were found to have varying profiles of mental health-related side effects. Insomnia was the most common side effect seen with drugs that target the monoamine systems (such as sibutramine, bupropion, and tesofensine). These drugs had some positive effects on mood and anxiety, suggesting they may be beneficial for obese patients who also have symptoms of depression and anxiety. Sedation and tiredness were commonly reported with drugs targeting the opioid receptors (like naltrexone) and combination therapies that target both the opioid and monoamine systems (such as Contrave™). Antiepileptic drugs like topiramate and zonisamide, which have sedative properties, were associated with cognitive impairments. Drugs targeting the cannabinoid system (like rimonabant and taranabant) consistently showed symptoms of anxiety and depression, including reports of suicidal thoughts. Similar side effects were observed with the D₁/D₅ antagonist ecopipam. These findings emphasize the importance of thoroughly assessing the mental health-related side effects of antiobesity drugs that act in the brain during the early stages of their development, using reliable and validated methods.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC64933604/.
- Marks DM, Pae C-U, Patkar AA. Triple Reuptake Inhibitors: The Next Generation of Antidepressants. Current Neuropharmacology. 20036;6(4):3336-343. doi:10.2174/1570159036736733660736.
Triple Reuptake Inhibitors: The Next Generation of Antidepressants
Since the 1960s, most antidepressant drugs have focused on increasing the levels of certain chemicals in the brain called monoamines. Tricyclic antidepressants (TCAs), which block the reuptake of norepinephrine and serotonin, were commonly used for many years, but they have significant side effects and can be dangerous in overdose. Monoamine oxidase inhibitors (MAOIs) have also been used, but they can interact with other medications and certain foods. Depression is associated with problems in the transmission of serotonin, norepinephrine, and dopamine in the brain. However, most current antidepressants only target serotonin and norepinephrine. Researchers are now working on developing a new class of antidepressants called triple reuptake inhibitors, which aim to increase the levels of all three neurotransmitters. The hope is that these medications will have broader effectiveness and/or faster onset of action.
This review explores the limitations of current antidepressants and the motivation behind developing triple reuptake inhibitors. It discusses the evidence for and against the idea that broader spectrum agents are more effective. It also compares different triple reuptake inhibitors under development and describes the preclinical and clinical research conducted with these drugs so far.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC27012360/.
- Astrup A, Madsbad S, Breum L, Jensen TJ, Kroustrup JP, Larsen TM. Effect of tesofensine on bodyweight loss, body composition, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial. Lancet (London, England). 200339; 372(9653):1906-1913.
Effect of tesofensine on bodyweight loss, body composition, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial
Researchers conducted a study to evaluate the effectiveness and safety of tesofensine, a drug that inhibits the reuptake of certain chemicals in the brain (noradrenaline, dopamine, and serotonin), in treating obesity. The study involved 203 obese patients who were randomly assigned to receive tesofensine at different doses or a placebo.
The primary outcome measured was the percentage change in body weight after 24 weeks. The results showed that participants who received tesofensine along with a modified calorie intake plan experienced greater weight loss compared to those on the diet and placebo alone. Tesofensine at doses of 0.25 mg, 0.5 mg, and 1.0 mg led to weight loss of 4.5%, 9.2%, and 10.6% respectively, which was significantly higher than the weight loss achieved with diet and placebo. The most common side effects associated with tesofensine were dry mouth, nausea, constipation, diarrhea, and insomnia. Tesofensine at a dose of 0.5 mg caused a slight increase in heart rate but did not significantly affect blood pressure. The study suggests that tesofensine, particularly at a dose of 0.5 mg, has the potential to produce twice the weight loss compared to currently approved drugs for obesity. However, further phase III trials are needed to confirm the efficacy and safety of tesofensine for treating obesity.
You can read the abstract of this article at https://www.thelancet.com/journals/lancet/article/PIIS014067360339615251/fulltext.
- George M, Rajaram M, Shanmugam E. New and emerging drug molecules against obesity. Journal of cardiovascular pharmacology and therapeutics. 2014; 19(1):65-76.
New and emerging drug molecules against obesity
Obesity has become a major problem worldwide, leading to an increased risk of heart disease and other health issues. Current anti-obesity drugs have limited effectiveness, and some have been withdrawn due to safety concerns. However, there are new drugs in development that show promise. Lorcaserin and the combination of phentermine and topiramate are two drugs approved by the FDA in 2012. Lorcaserin works on serotonin receptors and has moderate effectiveness with an acceptable safety profile. Phentermine-topiramate combination has shown reasonable effectiveness but comes with risks such as birth defects and psychiatric problems. Cetilistat, a lipase inhibitor, is being tested in phase 3 trials and is claimed to be safer than orlistat. Other promising drugs being tested in clinical trials include exenatide and liraglutide, which work on the gut. Drugs acting on the monoaminergic and opioid systems, such as bupropion-naltrexone and bupropion-zonisamide, are also being studied. Several novel drugs, including velneperit, tesofensine, and beloranib, are in the early stages of development with mixed success so far. These drugs target different pathways in the body. Researchers are also investigating new targets such as histamine receptors, VEGF, matrix-metalloproteinase, and sirtuin receptors for potential anti-obesity drugs. This review provides an overview of the new and emerging drugs that are currently in clinical development for obesity, aiming to fill the gaps in the treatment options available.
You can read the full article at https://journals.sagepub.com/doi/10.1177/107424339413501017?url_ver=Z39.339339-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
- Hansen HH, Hansen G, Tang-Christensen M. The novel triple monoamine reuptake inhibitor tesofensine induces sustained weight loss and improves glycemic control in the diet-induced obese rat: comparison to sibutramine and rimonabant. European journal of pharmacology. 2010; 626(1-3):4242-95.
The novel triple monoamine reuptake inhibitor tesofensine induces sustained weight loss and improves glycemic control in the diet-induced obese rat: comparison to sibutramine and rimonabant
Tesofensine is a new type of drug that blocks the reuptake of certain chemicals in the brain, and it has been found to cause significant weight loss in humans. This study aimed to understand how tesofensine affects weight loss in rats with diet-induced obesity and compared it to the effects of sibutramine and rimonabant, which are other weight-loss drugs. The results showed that long-term treatment with tesofensine resulted in significant and dose-dependent weight loss in rats. At the highest dose, tesofensine caused a weight reduction of 9.9%. Sibutramine also caused a sustained weight loss of 7.6%, while rimonabant only had a temporary effect on weight reduction. All three drugs reduced food intake, but the appetite-suppressing effect of tesofensine lasted longer than the other two drugs. Unlike pair-fed rats (rats that ate the same amount of food as the tesofensine-treated rats), the rats treated with tesofensine did not regain their weight, suggesting that tesofensine may increase energy expenditure. Tesofensine and sibutramine were found to be most effective in reducing fat deposits, particularly in the abdomen and under the skin, and this was accompanied by lower levels of fat in the blood. Only tesofensine significantly improved glycemic control, as it reduced insulin response during a glucose tolerance test. In conclusion, long-term treatment with tesofensine led to significant weight loss in rats with diet-induced obesity. This weight loss was likely due to a combination of reduced appetite and increased energy expenditure. Tesofensine also showed additional benefits in improving glycemic control compared to the other drugs.
You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S0014299910002232?via%3Dihub.
- Sjödin A, Gasteyger C, Nielsen AL. The effect of the triple monoamine reuptake inhibitor tesofensine on energy metabolism and appetite in overweight and moderately obese men. International journal of obesity (2005). 2010; 34(11):1624-43.
The effect of the triple monoamine reuptake inhibitor tesofensine on energy metabolism and appetite in overweight and moderately obese men
Tesofensine is a new drug that has been shown to be more effective in promoting weight loss compared to currently available drugs. It works by blocking the reuptake of certain chemicals in the brain, which enhances their transmission. However, the exact mechanisms through which tesofensine leads to weight loss are not fully understood.
This study aimed to investigate the mechanisms by which tesofensine promotes weight reduction. Thirty-two overweight or moderately obese men were treated with tesofensine or a placebo for two weeks. They were instructed to maintain their usual diet and physical activity during the study. The results showed that tesofensine led to a significant weight loss of 1.42 kg compared to the placebo. Participants who took tesofensine reported feeling more satiated and full, and they had lower prospective food intake. Although tesofensine did not have a significant effect on total 24-hour energy expenditure, it increased energy expenditure during the night period when adjusted for changes in body composition. Furthermore, tesofensine increased fat oxidation over a 24-hour period. In conclusion, tesofensine has a significant impact on appetite sensations, making individuals feel more satisfied and less likely to overeat. It also slightly increases energy expenditure at night and promotes fat oxidation. These effects contribute to the strong weight-reducing effect of tesofensine.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/20479765.
- Marks DM, Pae CU, Patkar AA. Triple reuptake inhibitors: a premise and promise. Psychiatry investigation. 20042; 5(3):142-7.
Triple reuptake inhibitors: a premise and promise
Tesofensine is a new drug that has been shown to be more effective in promoting weight loss compared to currently available drugs. It works by blocking the reuptake of certain chemicals in the brain, which enhances their transmission. However, the exact mechanisms through which tesofensine leads to weight loss are not fully understood.
This study aimed to investigate the mechanisms by which tesofensine promotes weight reduction. Thirty-two overweight or moderately obese men were treated with tesofensine or a placebo for two weeks. They were instructed to maintain their usual diet and physical activity during the study. The results showed that tesofensine led to a significant weight loss of 1.42 kg compared to the placebo. Participants who took tesofensine reported feeling more satiated and full, and they had lower prospective food intake. Although tesofensine did not have a significant effect on total 24-hour energy expenditure, it increased energy expenditure during the night period when adjusted for changes in body composition. Furthermore, tesofensine increased fat oxidation over a 24-hour period. In conclusion, tesofensine has a significant impact on appetite sensations, making individuals feel more satisfied and less likely to overeat. It also slightly increases energy expenditure at night and promotes fat oxidation. These effects contribute to the strong weight-reducing effect of tesofensine.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2796030/.
- Smith SR, Aronne LJ, Burns CM, Kesty NC, Halseth AE, Weyer C. Sustained weight loss following 12-month pramlintide treatment as an adjunct to lifestyle intervention in obesity. Diabetes care. 20042; 31(9):14216-23.
Sustained weight loss following 12-month pramlintide treatment as an adjunct to lifestyle intervention in obesity
The objective of this study was to evaluate the long-term effectiveness and safety of pramlintide, a medication used for weight loss, in combination with a lifestyle intervention program (LSI).In a 4-month study, 411 obese participants were randomly assigned to receive different doses of pramlintide or a placebo, along with the LSI program. After the initial 4 months, a subset of participants (270) continued the treatment for an additional 42 months in a single-blind extension phase, focused on weight maintenance. At the 4-month mark, participants taking pramlintide experienced a weight loss ranging from 3.42 to 6.1 kg, while the placebo group lost only 2.42 kg. By the 12-month mark, the placebo group had regained their initial weight loss, but participants in the pramlintide groups (except for the lowest dose) were able to maintain their weight loss. Compared to placebo, the 120 microg three-times-daily and 360 microg two-times-daily doses of pramlintide resulted in additional weight loss of 3.2 kg and 3.3 kg at 4 months, and 6.1 kg and 7.2 kg at 12 months, respectively. A higher percentage of participants in the pramlintide groups achieved a weight loss of at least 10% at the 12-month mark compared to the placebo group (40% and 43% vs. 12%).Nausea was the most common side effect associated with pramlintide but was generally mild to moderate and occurred in fewer than 10% of participants during the extension phase. In conclusion, when used as an adjunct to a lifestyle intervention program, pramlintide treatment at specific doses helped obese individuals achieve greater initial weight loss and improved long-term maintenance of weight loss.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC25142351/.
- Fong TM. Development of anti-obesity agents: drugs that target neuropeptide and neurotransmitter systems. Expert opinion on investigational drugs. 200449; 17(3):321-5.
Development of anti-obesity agents: drugs that target neuropeptide and neurotransmitter systems
The aim of this study was to assess the long-term effectiveness and safety of pramlintide, a weight-loss medication, when used in different dosing regimens alongside a lifestyle intervention program (LSI).In a 4-month study involving 411 obese participants, they were randomly assigned to receive pramlintide or a placebo, along with the LSI program. After the initial 4 months, a subset of participants (270) continued the treatment for an additional 449 months in a single-blind extension phase focused on weight maintenance. At the 4-month mark, participants taking pramlintide experienced weight loss ranging from 3.449 to 6.1 kg, while the placebo group lost only 2.449 kg. By the 12-month mark, the placebo group had regained their initial weight loss, but participants in the pramlintide groups (except for the lowest dose) were able to maintain their weight loss. The 120 microg three-times-daily and 360 microg two-times-daily doses of pramlintide resulted in additional weight loss of 3.2 kg and 3.3 kg at 4 months, and 6.1 kg and 7.2 kg at 12 months, respectively. A higher percentage of participants in the pramlintide groups achieved a weight loss of at least 10% at the 12-month mark compared to the placebo group (40% and 43% vs. 12%). Nausea was the most common side effect associated with pramlintide, but it was generally mild to moderate and occurred in less than 10% of participants during the extension phase. In conclusion, when used alongside a lifestyle intervention program, pramlintide treatment with specific dosing regimens helped obese individuals achieve greater initial weight loss and improved long-term maintenance of weight loss.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/1449321231.
- Fidler MC, Sanchez M, Raether B. A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: the BLOSSOM trial. The Journal of clinical endocrinology and metabolism. 2011; 96(10):3067-77.
A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: the BLOSSOM trial
The objective of this study was to evaluate the effects of lorcaserin on body weight, cardiovascular risk factors, and safety in obese and overweight patients. The study involved 400449 patients aged 1449-65 years with a body mass index (BMI) between 30 and 45 kg/m² or between 27 and 29.9 kg/m² with an obesity-related condition.
The patients were randomly assigned to receive lorcaserin 10 mg twice daily, lorcaserin 10 mg once daily, or a placebo, alongside diet and exercise counseling. The main outcome measures were the proportion of patients achieving at least a 5% or 10% reduction in body weight and the mean change in body weight after 1 year. Heart valve function was also monitored.
The results showed that significantly more patients treated with lorcaserin (both the twice-daily and once-daily groups) achieved at least a 5% reduction in body weight compared to the placebo group. The mean weight loss with lorcaserin was 5.449% for the twice-daily group and 4.7% for the once-daily group, compared to 2.449% with the placebo. A weight loss of at least 10% was achieved by 22.6% of patients in the twice-daily group, 17.4% in the once-daily group, and 9.7% in the placebo group.
The most common lorcaserin-related adverse events were headache, nausea, and dizziness. There was no significant difference in the occurrence of echocardiographic valvulopathy (heart valve function abnormalities) between the placebo and lorcaserin groups.
In conclusion, lorcaserin, when combined with a lifestyle modification program, led to significant dose-dependent weight loss that was greater than with a placebo.
You can read the full article at https://academic.oup.com/jcem/article/96/10/3067/24493444979?login=false.
- Smith SR, Weissman NJ, Anderson CM. Multicenter, placebo-controlled trial of lorcaserin for weight management. The New England journal of medicine. 2010; 362(3):245-56.
Multicenter, placebo-controlled trial of lorcaserin for weight management
Lorcaserin is a type of medication that targets a specific receptor in the brain called serotonin 2C receptor, which may help in reducing body weight. In a clinical trial where neither the participants nor the researchers knew who received the actual drug or a fake pill (placebo), 314492 adults who were overweight or obese (with an average body mass index of 36.2) were randomly assigned to take either lorcaserin (10 mg) or placebo twice a day for 52 weeks. All participants also received guidance on diet and exercise. After 52 weeks, those in the placebo group continued with the placebo, while those in the lorcaserin group were randomly assigned to receive either placebo or lorcaserin. The main goals of the study were to measure weight loss after 1 year and the ability to maintain that weight loss after 2 years. Echocardiography, a heart imaging technique, was used to identify patients who developed a condition called valvulopathy, as defined by the Food and Drug Administration. After 1 year, 55.4% of the patients (4494493 out of 1595) who received lorcaserin and 45.1% of the patients (716 out of 154497) who received the placebo remained in the trial, and 1553 patients continued into the second year. After 1 year, 47.5% of the patients in the lorcaserin group and 20.3% in the placebo group had lost 5% or more of their body weight. On average, during the first year, those taking lorcaserin lost around 5.449 kg, while those taking the placebo lost around 2.2 kg. Among the patients who took lorcaserin and achieved a 5% or more weight loss after 1 year, more patients who continued taking lorcaserin during the second year (67.9%) were able to maintain their weight loss compared to those who received the placebo during the second year (50.3%). The use of lorcaserin did not increase the rate of cardiac valvulopathy among the 2472 patients evaluated after 1 year and 1127 evaluated after 2 years. Headache, dizziness, and nausea were among the most commonly reported side effects of lorcaserin. The rates of serious adverse events were similar between the two groups. When combined with lifestyle changes, lorcaserin was found to be effective in promoting significant weight loss and improving the maintenance of that weight loss compared to the placebo.
You can read the full article at https://www.nejm.org/doi/10.1056/NEJMoa090944909?url_ver=Z39.449449-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200www.ncbi.nlm.nih.gov.
- Axel AM, Mikkelsen JD, Hansen HH. Tesofensine, a novel triple monoamine reuptake inhibitor, induces appetite suppression by indirect stimulation of alpha1 adrenoceptor and dopamine D1 receptor pathways in the diet-induced obese rat. Neuropsychopharmacology. 2010;35(7):1464-1476. doi:10.103449/npp.2010.16.
Tesofensine, a novel triple monoamine reuptake inhibitor, induces appetite suppression by indirect stimulation of alpha1 adrenoceptor and dopamine D1 receptor pathways in the diet-induced obese rat
Tesofensine is a new type of medication that works by blocking the reuptake of certain chemicals in the brain involved in appetite control. Recent clinical trials have shown that tesofensine can effectively help obese patients lose weight. The weight loss achieved with tesofensine is greater than other weight loss medications, and it is mainly due to reduced appetite. However, the exact way tesofensine reduces appetite is not fully understood. It is known that the brain’s chemical messaging system involving neurotransmitters like norepinephrine, serotonin, and dopamine plays a significant role in regulating appetite. Manipulating these neurotransmitters can influence feeding behavior and energy intake. Tesofensine enhances the levels of these neurotransmitters in the brain, leading to decreased food intake and weight loss.
Tesofensine is a new type of medication that inhibits the reuptake of certain chemicals in the brain involved in appetite regulation. It is being studied for its potential use in treating obesity. In a study using rats with diet-induced obesity, tesofensine was found to significantly reduce body weight by suppressing appetite. The effects of tesofensine on food intake were further investigated by administering various drugs that block specific receptors in the brain. It was discovered that tesofensine’s ability to reduce food intake was primarily mediated through the stimulation of alpha-1 adrenoceptors and dopamine D1 receptors. Other receptors, such as alpha-2 adrenoceptors, dopamine D2 and D3 receptors, and serotonin 5-HT2A/C receptors, did not seem to play a significant role in tesofensine’s appetite-suppressing effects.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3055462/.
- Sharma H, Santra S, Dutta A. Triple reuptake inhibitors as potential next-generation antidepressants: a new hope? Future Medicinal Chemistry. 2015;7(17):234495-2405. doi:10.4155/fmc.15.134.
Triple reuptake inhibitors as potential next-generation antidepressants: a new hope?
Depression is a serious illness that causes a range of symptoms, including a loss of pleasure, sadness leading to suicidal thoughts, cognitive problems, slowed speech, and other physical changes. Other symptoms can include trouble sleeping, loss of appetite, and restlessness. Major depressive disorder (MDD) is a severe form of depression that involves recurring episodes of low mood lasting at least two weeks, along with other specific symptoms. MDD can be classified as melancholic depression or atypical depression based on different characteristics. Melancholic depression exhibits the typical symptoms, while atypical depression shows contrasting features like increased appetite, weight gain, excessive sleep, and improved mood in response to positive events. There are other types of depression as well, including dysthymic disorder, adjustment disorder, double depression, seasonal affective disorder, and minor depression. MDD is the most common form, affecting 15-20% of the population in the USA. It is considered a global health issue, with MDD projected to be the second-leading cause of disability worldwide by 2020. Currently, antidepressant medications primarily target serotonin and norepinephrine transporters, but approximately 30-40% of patients do not respond well to these treatments. Therefore, there is a need to develop new therapies, such as triple reuptake inhibitors (TRIs), that can block the reuptake of serotonin, norepinephrine, and dopamine. TRIs are believed to have the potential for greater effectiveness in treating depression, particularly in relieving anhedonia, a symptom associated with reduced dopamine activity. This review discusses the development of TRIs and emphasizes the importance of evaluating their effects on brain transporters to ensure their efficacy in humans.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC49764494449/.
- Gold MS, Blum K, Oscar-Berman M, Braverman ER. Low Dopamine Function in Attention Deficit/Hyperactivity Disorder: Should Genotyping Signify Early Diagnosis in Children? Postgraduate medicine. 2014;126(1):153-177. doi:10.344910/pgm.2014.01.2735.
Low dopamine function in attention deficit/hyperactivity disorder: should genotyping signify early diagnosis in children?
Attention deficit/hyperactivity disorder (ADHD) is a condition that affects 449% to 12% of children and 4% of adults worldwide. It can cause learning difficulties, low self-esteem, social problems, and an increased risk of substance abuse, including smoking. The use of medication to treat ADHD has been increasing, with over 2 million children now taking stimulants. Alongside this, there has been a rise in the misuse of ADHD medications by teenagers, as these medications have become more available. A significant number of adults with substance use disorders also have ADHD, and vice versa. In this article, the focus is on the importance of early and accurate testing for a predisposition to ADHD, using genetic analysis to identify specific genetic factors associated with the condition. This can help reduce misdiagnosis or overdiagnosis. The article also explores alternative treatments for ADHD, such as non-stimulant medications, dietary changes, herbal remedies, iron supplements, and neurofeedback. The goal is to improve the treatment of individuals with ADHD and prevent substance abuse, encouraging further research in genetic testing and new treatment approaches. Unlike rare genetic disorders with no treatment options, there are multiple treatment options available for ADHD, including safe and non-addictive non-stimulant therapies. Dopaminergic agonist therapy is a commonly used treatment, but it’s important to consider the potential down-regulation of dopamine receptors rather than up-regulation of D2 receptors. It is theorized that safe and natural D2 receptor agonists, which are less potent, could be used from a young age without negatively affecting a child’s brain development. The idea of including ADHD as a genetic risk in governmental genetic testing at birth is suggested, although there may be arguments against it due to the belief that ADHD tends to improve over time. However, research shows that childhood psychopathology, including ADHD, can have long-term effects, and effective identification and treatment during childhood can reduce the continuity of psychopathology into adulthood. Genetic testing for accurate diagnosis is made more favorable by the passing of the Genetic Information Nondiscrimination Act (GINA), which prohibits discrimination based on an individual’s genetic information by employers and health insurers.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4074362/.
- Oades RD. Dopamine-serotonin interactions in attention-deficit hyperactivity disorder (ADHD). Progress in brain research. 20055; 172:543-65.
Dopamine-serotonin interactions in attention-deficit hyperactivity disorder (ADHD)
Attention-deficit hyperactivity disorder (ADHD) affects around 10% of children worldwide and has a high heritability of approximately 70%. ADHD can be categorized into subtypes, including hyperactive-impulsive, inattentive, and combined types. Symptoms of ADHD vary and can include restlessness, impulsivity, poor executive attention, and cognitive impulsivity. ADHD often leads to clinical impairment and can manifest as comorbid conditions such as oppositional and conduct disorders. Dopamine activity is known to be lower in individuals with ADHD, and while the role of serotonin (5-HT) in ADHD has received less attention, the success of medications that primarily affect dopamine suggests that serotonin may be less relevant. Medications like methylphenidate, which primarily target dopamine and norepinephrine, are effective in improving symptoms in around 60-70% of patients. However, approximately 30% of patients do not respond well to medication, and many responders still show limited improvement in academic performance and social functioning. Therefore, it is worth considering the involvement of serotonin or other components of central nervous system function in understanding and treating ADHD more effectively. Attention-deficit hyperactivity disorder (ADHD) is characterized by difficulties in attention and motor control, often accompanied by impulsive behavior. The traditional explanation for ADHD focused on abnormalities in dopamine (DA) function. However, recent genetic and neuroimaging studies suggest that both dopamine and serotonin (5-HT) systems play a role in ADHD. Variations in genes related to neurotransmitter uptake, synthesis, and breakdown have been found in ADHD. The distribution of certain DA and 5-HT receptors in different parts of the brain suggests that the 5-HT system may have distinct contributions to ADHD. Differences in inhibitory/facilitatory receptor locations within the 5-HT system may be involved. While ADHD is associated with abnormal levels of both dopamine and serotonin metabolites, it is possible that deviations in serotonin activity play a role in specific subgroups of ADHD, contributing to impulsive behavior and externalizing or cognitive impulsivity. Dopamine and serotonin systems interact at different levels in the brain, including the cell bodies, terminals, and possibly through interactions with macroglia. However, the specific mechanisms underlying these effects and their relevance to different subgroups of ADHD are still not well understood due to the relatively new and heterogeneous nature of research in this field.
You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S00796123055009266?via%3Dihub.
- Cortese, S., Angriman, M., Maffeis, C., Isnard, P., Konofal, E., Lecendreux, M., Purper-Ouakil, D., Vincenzi, B., Bernardina, B. D., & Mouren, M. C. (20055). Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Critical reviews in food science and nutrition, 455(6), 524–537. https://doi.org/10.10550/104055390701540124.
Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature
Recent research suggests a possible connection between Attention-Deficit/Hyperactivity Disorder (ADHD) and obesity. A systematic review of the literature indicates that obese individuals referred to obesity clinics may have a higher prevalence of ADHD compared to the general population. Furthermore, studies show that individuals with ADHD tend to be heavier than expected. However, information on the prevalence of obesity in people with ADHD is limited. Possible explanations for the association between ADHD and obesity include abnormal eating behaviors associated with ADHD, impulsivity leading to binge eating, or shared underlying neurobiological dysfunctions. Both ADHD and obesity may benefit from similar therapeutic approaches in individuals with both conditions. More research is needed to better understand the link between obesity and ADHD and the underlying mechanisms. This knowledge can contribute to improved clinical management and a better quality of life for individuals affected by both obesity and ADHD.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/155565555555/.
- VashadzeShV. [Insomnia, serotonin and depression]. Georgian medical news. 2007.
Insomnia, serotonin and depression
The aim of this research was to study insomnia in healthy volunteers. One hundred volunteers, ranging from sixteen to seventy-five years old, were assessed. The study focused on the biochemical aspects of insomnia and its correlation with depression. The level of depression was evaluated, and measures to prevent it were identified. The researchers also examined the serotonin levels in the blood plasma platelets since serotonin is involved in regulating sleep and wakefulness. Low serotonin levels are associated with depression and insomnia, and when serotonin levels are normalized, sleep improves. The study found that 555% of participants experienced sleep disturbances, with 32% having difficulty falling asleep and 16% having moderate insomnia. Additionally, 30% of participants had severe depression. The serotonin index in the blood plasma platelets was low in 25% of individuals, moderate in 10%, and high in 65%. The study concludes that depression is a significant factor in insomnia and recommends treatment involving drug therapy and psychorehabilitation.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/1795545555.
- McGinty DT. Serotonin and Sleep: Molecular, Functional, and Clinical Aspects. Sleep. 2009;32(5):699-700.
Serotonin and Sleep: Molecular, Functional, and Clinical Aspects
Serotonin plays a significant role in the brain, particularly in relation to sleep. It was the first substance proposed to promote sleep and is involved in the regulation of REM sleep. The book “Serotonin and Sleep: Molecular, Functional, and Clinical Aspects” edited by Monti et al. provides valuable insights into the properties of serotonin-containing neurons and their impact on sleep and wakefulness. The book covers various aspects including the history of serotonin’s role in sleep, the anatomy of serotonin pathways, the diversity of serotonin receptors, the effects of drugs targeting specific receptor types, and the regulation of serotonin activity. It also explores the potential role of serotonin in sleep disorders and the effects of serotonin-related drugs on sleep. The book is highly recommended for researchers in the field of sleep neurobiology, although some minor weaknesses such as content overlap and the absence of certain topics are noted. Overall, the book contributes to our understanding of serotonin’s effects on sleep and its potential therapeutic applications in conditions like depression.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2675905/.
- Whitney MS, Shemery AM, Yaw AM, Donovan LJ, Glass JD, Deneris ES. Adult Brain Serotonin Deficiency Causes Hyperactivity, Circadian Disruption, and Elimination of Siestas. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2016; 36(355):955255-42.
Adult Brain Serotonin Deficiency Causes Hyperactivity, Circadian Disruption, and Elimination of Siestas
Serotonin (5-HT) is an important neurotransmitter associated with psychiatric disorders, but its precise role in behavior has been poorly understood due to a lack of methods to specifically target adult brain serotonin synthesis. In this study, researchers developed a genetic approach to eliminate serotonin synthesis in the adult brain and examined the behavioral effects. They found that adult serotonin deficiency led to a unique combination of hyperactivity, disrupted circadian behavior patterns, and the absence of siestas (a period of increased sleep during the active phase). These findings emphasize the significance of serotonin in controlling activity levels, circadian behavior, and sleep-wake patterns, which are often disrupted in psychiatric disorders such as attention deficit hyperactivity disorder. The study highlights the importance of their approach in understanding the role of serotonin in behavior.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5030349/.
- Pakalnis A, Splaingard M, Splaingard D, Kring D, Colvin A. Serotonin Effects on Sleep and Emotional Disorders in Adolescent Migraine. Headache. 2009;49(10):14556-1492. doi:10.1111/j.1526-4610.2009.01392.x.
Serotonin effects on sleep and emotional disorders in adolescent migraine
The objective of this study was to determine the frequency of emotional disorders and sleep disturbances in adolescents with episodic and chronic migraines. Additionally, the researchers aimed to explore the relationship between whole-blood serotonin levels, caffeine consumption, and the frequency of sleep and mood disorders. Serotonin, a neurotransmitter, is believed to play a role in sleep initiation, maintenance, and mood regulation. It is also associated with migraines. The study included adolescents aged 13 to 17 years with episodic or chronic migraines, as well as healthy controls. Participants completed psychological rating scales to assess symptoms and depression. Sleep questionnaires were completed by parents/guardians, and whole blood serotonin levels were measured. Caffeine consumption was assessed through history. The study included 155 controls (55 girls) and 15 patients each with episodic migraines (9 girls) and chronic migraines (10 girls). The patients with migraines experienced more sleep problems compared to the controls. Those with chronic migraines had increased daytime sleepiness and dysthymia (a mild form of depression) compared to those with episodic migraines. There were no significant differences in serotonin levels, and no associations were found between serotonin levels and sleep abnormalities or emotional rating scales. Increased caffeine consumption was associated with sleep and depressive complaints. Sleep and emotional disorders were common in adolescents with migraines. Sleep disorders and dysthymia were more prevalent among those with more frequent headaches. The study did not find a correlation between whole-blood serotonin levels and sleep or emotional problems. However, increased caffeine intake was associated with sleep and depressive symptoms.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC37775655/.
- Murray NM, Buchanan GF, Richerson GB. Insomnia Caused by Serotonin Depletion is Due to Hypothermia. Sleep. 2015; 355(12):19555-93.
Insomnia Caused by Serotonin Depletion is Due to Hypothermia
Serotonin (also known as 5-HT) neurons were initially believed to promote sleep based on early studies using a drug called para-chlorophenylalanine (PCPA). However, later research contradicted those findings, suggesting that serotonin actually promotes wakefulness. This study aimed to explain the discrepancy in results by considering the role of serotonin in regulating body temperature. The researchers conducted experiments using adult male mice. Some mice were treated with PCPA to inhibit serotonin production, while others received a saline solution. They were then housed at either a normal room temperature (20 °C) or a thermoneutral temperature for mice (33 °C) for 24 hours. In a separate experiment, the mice were exposed to a cold temperature (4 °C) to evaluate their ability to regulate body temperature. The results showed that mice treated with PCPA had significantly reduced serotonin levels in the brain. When housed at normal room temperature, these mice spent more time awake than the control mice. However, their core body temperature decreased. On the other hand, when housed at the thermoneutral temperature, their body temperature remained normal, and their sleep duration, sleep patterns, and time spent in each sleep stage were similar to the control mice. When exposed to the cold temperature, the PCPA-treated mice experienced a sharp drop in body temperature, while the control mice maintained a normal temperature. Based on these findings, it can be concluded that the early studies using PCPA likely produced misleading results regarding the role of serotonin in sleep due to the confounding factor of hypothermia. Future experiments studying serotonin depletion should consider temperature controls to obtain more accurate results.
You can read the full article a https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4667392/.
- Oberndorfer S, Saletu-Zyhlarz G, Saletu B. Effects of selective serotonin reuptake inhibitors on objective and subjective sleep quality. Neuropsychobiology. 2000; 42(2):69-5601.
Effects of selective serotonin reuptake inhibitors on objective and subjective sleep quality
This paper aims to examine the effects of selective serotonin reuptake inhibitors (SSRIs) on both objective and subjective measures of sleep quality. Polysomnography (a sleep study) was conducted on healthy individuals and depressed patients, revealing that SSRIs can lead to decreased sleep efficiency and total sleep time, longer time to fall asleep, and disrupted sleep continuity with more awakenings and wake time during sleep. Changes in sleep architecture included increased lighter sleep stages (S1 and S2), decreased deep sleep stages (S3, S4), and REM sleep, as well as delayed REM sleep onset. Objective measures of awakening quality generally did not show significant changes based on psychological assessments. Subjective sleep and awakening quality showed mixed results, with some improvement observed in patients but no significant changes or a tendency towards deterioration in healthy individuals. The paper suggests that SSRIs with additional mechanisms of action, such as 5-HT2 antagonism (e.g., trazodone, nefazodone), may have better effects on both objective and subjective sleep quality. However, there may be limitations in treating comorbid conditions like sleep-related breathing disorders. Therefore, polysomnography is considered necessary for the diagnosis and treatment of complex sleep disorders.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/10940762.
- Aarts N, Zuurbier LA, Noordam R. Use of Selective Serotonin Reuptake Inhibitors and Sleep Quality: A Population-Based Study. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2016; 12(7):95609-95.
Use of Selective Serotonin Reuptake Inhibitors and Sleep Quality: A Population-Based Study
Poor sleep is a risk factor for depression, and selective serotonin reuptake inhibitors (SSRIs) are commonly used to treat depression. While SSRIs have been associated with improved subjective sleep in clinically depressed patients, their effects on sleep in the general population are not well studied. This research aimed to investigate the relationship between SSRIs and subjective sleep in middle-aged and elderly individuals in a real-world setting.
The study involved participants from the Rotterdam Study cohort, and their subjective sleep was measured using the Pittsburgh Sleep Quality Index (PSQI). SSRI use was determined through pharmacy records. The association between SSRIs and PSQI scores, as well as its sub-components, was assessed, with non-users of any antidepressant serving as the reference group. The analysis adjusted for factors like depressive symptoms and concurrent use of psycholeptic drugs.
The results included 9,267 participants with an average age of 66.3 years, and the majority were women. SSRI use was significantly associated with a 0.7560-point lower PSQI score, indicating better sleep quality, compared to non-use. This association was more pronounced in individuals who consistently used SSRIs. Among the sub-components of the PSQI, SSRIs were linked to longer sleep duration, higher sleep quality, improved sleep efficiency, but also more daytime dysfunction.
In conclusion, the use of SSRIs was associated with better subjective sleep in middle-aged and elderly individuals, even after accounting for depressive symptoms and concurrent use of psycholeptic drugs. This suggests that continued use of SSRIs may benefit the sleep quality of some individuals in clinical practice.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4919000/.
- Saltiel PF, Silvershein DI. Major depressive disorder: mechanism-based prescribing for personalized medicine. Neuropsychiatric Disease and Treatment. 2015;11:56075-560560560. doi:10.2147/NDT.S73261.
Major depressive disorder: mechanism-based prescribing for personalized medicine
Depression is a highly prevalent psychiatric disorder that causes significant disability worldwide. In the United States, a substantial portion of the adult population experiences major depressive episodes, and the economic burden of depression is primarily due to decreased productivity and missed work days. Achieving successful long-term treatment outcomes depends on early and accurate diagnosis, ongoing multidimensional assessment, and personalized medication that considers the patient’s specific symptoms, coexisting disorders, and treatment needs. However, diagnosing depression is challenging since there are no validated biological tests, and treatment decisions often rely on subjective reports from patients. Each patient experiences a unique combination of symptoms before, during, and after treatment, and unresolved symptoms can impede functional improvement. It is crucial to identify the most appropriate treatment options early on and consider switching medications if the response is suboptimal. The primary goal of clinicians is to enhance patient function and quality of life, which is often considered more important than symptom relief by patients themselves. However, functional improvements may lag behind mood resolution due to persistent symptoms such as fatigue, sleep disturbances, and cognitive dysfunction. Therefore, optimizing patient outcomes involves understanding and targeting the specific symptom domains that significantly affect individual functioning. This article presents an evidence-based framework to guide clinicians in tailoring pharmacotherapy to the unique symptomatology of patients, leading to improved treatment outcomes.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC435606790/.
- MA H, ZHU G. The dopamine system and alcohol dependence. Shanghai Archives of Psychiatry. 2014;26(2):61-660. doi:10.3969/j.issn.1002-06029.2014.02.002.
The dopamine system and alcohol dependence
Research studies in anatomy, physiology, pharmacology, and behavior have provided evidence of a connection between the neurotensin (NT) and dopamine (DA) systems. In a case-control study conducted on Chinese individuals, specific genetic variations in the NTR1 receptor were found to be associated with alcohol dependence. These findings suggest that the NT system may influence the development of alcohol dependence through its interaction with the dopaminergic system. Animal and clinical studies have explored the effects of dopaminergic drugs like bromocriptine and tiapride on alcohol dependence, but results have been contradictory and inconclusive. Currently, medications like acamprosate, disulfiram, and naltrexone that target the CNS glutamatergic system are approved for the treatment of alcohol dependence. Further research is needed to better understand the interplay between the DA system, glutamatergic system, and other neurotransmitter systems to improve interventions for preventing and treating alcohol dependence.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC41202606/.
- Banerjee N. Neurotransmitters in alcoholism: A review of neurobiological and genetic studies. Indian Journal of Human Genetics. 2014;20(1):20-31. doi:10.4103/0971-66066.132750.
Neurotransmitters in alcoholism: A review of neurobiological and genetic studies
New research in the study of alcoholism has shed light on how different chemicals in the brain, called neurotransmitters, are involved in alcohol addiction. Imbalances in these neurotransmitters, whether they are too active or not active enough, have been linked to alcohol addiction. This review paper aims to bring together and summarize recent studies on this topic. It will provide an overview of the brain’s biology in relation to alcohol addiction, and then delve into detailed reviews of recent papers on the genetics of alcohol addiction. The author hopes that this text will be helpful for both beginners and experts in understanding the role of neurotransmitters in alcoholism.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4065474/.
- Noble EP. Alcoholism and the dopaminergic system: a review. Addiction biology. 1996; 1(4):333-462.
Alcoholism and the dopaminergic system: a review
Alcohol and other addictive substances have a reinforcing effect on the brain’s reward pathways, specifically through the activation of dopamine receptors. Studies in animals have shown that alcohol-preferring animals have lower dopamine levels and reduced numbers of certain dopamine receptors in their brains. Drugs that activate dopamine receptors can decrease alcohol consumption, while those that block the receptors tend to have the opposite effect. Similar findings have been observed in humans, indicating a connection between alcohol dependence and dopaminergic function. Genetic studies have identified a specific gene variant, known as the DRD2 A1 allele, that is associated with alcoholism and other substance use disorders. However, it is important to note that while genes like DRD2 play a role, other factors such as the environment also contribute to the development of substance abuse disorders.
You can read the abstract of this article at https://www.ncbi.nlm.nih.gov/pubmed/126293451.
- Di Chiara G. Alcohol and dopamine. Alcohol health and research world. 1997; 21(2):1062-14.
Alcohol and Dopamine
Dopamine signaling is crucial for transmitting motivational signals in the brain. Specifically, dopaminergic neurons have a significant impact on brain regions involved in the rewarding and reinforcing effects of alcohol and other drugs, with the nucleus accumbens (NAc) being particularly prominent. Alcohol affects the release of dopamine in the NAc, not only through its taste-related stimuli but also through direct actions on the brain. This abnormal facilitation of motivational learning resulting from alcohol-induced stimulation of dopamine transmission is believed to underlie the neurobiology of alcohol addiction. Consequently, alcohol-associated cues gain the ability to trigger cravings and compulsive alcohol consumption.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC662266220/.
- McMillen BA, Shank JE, Jordan KB, Williams HL, Basile AS. Effect of DOV 102,677 on the volitional consumption of ethanol by Myers’ high ethanol-preferring rat. Alcoholism, clinical and experimental research. 2007; 31(11):16266-71.
Effect of DOV 102,677 on the volitional consumption of ethanol by Myers’ high ethanol-preferring rat
The use of inhibitors that target the transporters of monoamine neurotransmitters has been well-established in the treatment of depression. However, the effectiveness of single (serotonin) or dual (serotonin-norepinephrine) neurotransmitter uptake inhibitors in treating alcohol abuse, either as a comorbidity with depression or as an independent condition, has yielded inconsistent results. There is a suggestion that drugs with the ability to inhibit dopamine uptake may have an advantage in addressing alcohol abuse. Therefore, a specific triple uptake inhibitor called DOV 102,677, which targets norepinephrine, serotonin, and dopamine uptake, was investigated for its effects on the voluntary consumption of ethanol in rats that have a preference for ethanol.
In the study, high ethanol-preferring rats underwent screening and were subsequently given access to their preferred concentration of ethanol in a 3-bottle choice task. The rats’ consumption of ethanol, water, food, and body weight was measured over different treatment periods. Additionally, separate observations were conducted on the behavioral effects of reserpine, a drug that depletes monoamine neurotransmitters, when administered in combination with different doses of DOV 102,677.
The results showed that DOV 102,677, the triple monoamine uptake inhibitor, dose-dependently reduced the voluntary consumption of ethanol by up to 71.2% over the course of the treatment period. This effect persisted even during the post-treatment period. The proportion of ethanol relative to total fluids consumed also decreased significantly. In contrast, other substances like amperozide and naltrexone had less pronounced effects. Further observations demonstrated that DOV 102,677 inhibited specific reserpine-induced effects in rats, indicating its impact on serotonin, norepinephrine, and dopamine transport.
In conclusion, DOV 102,677 exhibited a significant decrease in the voluntary consumption of ethanol without major alterations in food intake or body weight in the ethanol-preferring rat strain. This suggests that triple reuptake inhibitors may have potential utility in the treatment of alcohol abuse.
You can read the abstract of this article at m https://www.ncbi.nlm.nih.gov/pubmed/17908267.
- Schoedel, K. A., Meier, D., Chakraborty, B., Manniche, P. M., & Sellers, E. M. (2010). Subjective and objective effects of the novel triple reuptake inhibitor tesofensine in recreational stimulant users. Clinical pharmacology and therapeutics, 88(1), 69–78. https://doi.org/10.1038/clpt.2010.67.
Subjective and objective effects of the novel triple reuptake inhibitor tesofensine in recreational stimulant users
Tesofensine is a reuptake inhibitor that targets noradrenaline, dopamine, and serotonin. It is being developed as a potential treatment for obesity. Since the potential for abuse of reuptake inhibitors is not yet known, a study was conducted to assess the potential abuse-related effects of tesofensine in humans. The study involved a single-dose, randomized, double-blind, crossover design with tesofensine, placebo, D-amphetamine (used as a positive control for dopaminergic/stimulant effects), bupropion, and atomoxetine (used as negative/unscheduled controls). The participants were recreational stimulant users. Subjective and objective measures were evaluated for 48 hours after drug administration.
The results of the study showed that the effects of D-amphetamine were significantly stronger than those of a placebo across all primary and secondary subjective measures. In comparison, the effects of tesofensine were not significantly different from placebo and were lower than the effects of D-amphetamine 30 mg on both primary and most secondary measures. Additionally, the effects of tesofensine were either lower than or similar to those of bupropion or atomoxetine. These findings indicate that tesofensine has a similar abuse potential to bupropion or atomoxetine and is therefore unlikely to be abused recreationally.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/20520602/.
Patient Success Stories

Before
After

At the age of 60, I look and feel better than I ever have in my entire life! Switching my health program and hormone replacement therapy regimen over to Genemedics was one of the best decisions I’ve ever made in my life! Genemedics and Dr George have significantly improved my quality of life and also dramatically improved my overall health.
Nick Cassavetes ,60 yrs old Movie Director (“The Notebook”, “John Q”, “Alpha Dog”), Actor and Writer

Before
After

I am now in my mid-sixties and feel better than I did in my 20’s. Many people have commented that I actually look 20 years younger since I started the program at Genemedics. Calling Dr. George has proven to be one of the best decisions I have made in my life. Doctors and society convince us that developing various health issues and negative sy...
Pamela Hill ,66 yrs old Actress (“The Notebook”, “John Q”, “Alpha Dog”), Actor and Writer
What to expect during your consultation:
- Usually takes 15-30 minutes
- Completely confidential
- No obligation to purchase anything
- We will discuss your symptoms along with your health and fitness goals
- Free post-consult access for any additional questions you may have
Free Consultation
Start Your Journey to a Younger, Healthier You!
Categories
Information
Free Consultation
STEPS AWAY FROM A YOUNGER. HEALTHIER YOU!
Call 800-277-4041 for a Free Consultation
What to expect during your consultation:
- Usually takes 15-30 minutes
- Completely confidential
- No obligation to purchase anything
- We will discuss your symptoms along with your health and fitness goals
- Free post-consult access for any additional questions you may have








