GENEMEDICS APP
GENEMEDICS NUTRITION
Aminophylline
Author: Dr. George Shanlikian, M.D. | Last Updated: January 27th, 2024
- Home
- >
- Health Library
- >
- Aminophylline
- 5-amino-1MQ
- Aminophylline
- Aniracetam
- ARA 290
- Argireline + Leuphasyl
- BPC-157
- Bremelanotide
- Cerebrolysin
- CJC-1295
- Delta Sleep-Inducing Peptide
- Dihexa
- Elampretide (SS-31)
- Epithalon
- FG Loop Peptide (FGL)
- GHK-Cu
- Ginsenoside Rg3
- Glycyrrhetinic Acid
- Ipamorelin
- Kisspeptin
- KPV
- LL-37
- Melanotan 1
- Melanotan 2
- Mitochondrial ORF of the twelve S c (MOTS-c)
- MK-677 (IBUTAMOREN)
- Nicotinamide Adenine Dinucleotide (NAD+)
- Nicotinamide Riboside
- NMN (Nicotinamide Mononucleotide)
- Noopept
- Pegylated Mechano Growth Factor
- Selank
- Semax
- Sermorelin
- SRT2104
- Tesamorelin
- Thymosin Alpha 1
- Thymosin Beta 4
- Tiger 17
- Valproic Acid
- Valproic acid + PTD-DBM
- Vasoactive Intestinal Peptide
- Zinc-Thymulin
- Potential Benefits of Aminophylline
- Key Takeaways of Aminophylline
- What is Aminophylline?
- Aminophylline Mechanism of Action
- Chemical Structure of Aminophylline
- Research on Aminophylline
- Aminophylline Uses
- Aminophylline Contraindications
- Associated Side Effects of Aminophylline
- Aminophylline Dosage
- Aminophylline vs Theophylline
- Aminophylline Before and After
- FAQs
- Aminophylline References
Book a Free Consultation
Table of Contents
- Potential Benefits of Aminophylline
- Key Takeaways of Aminophylline
- What is Aminophylline?
- Aminophylline Mechanism of Action
- Chemical Structure of Aminophylline
- Research on Aminophylline
- Aminophylline Uses
- Aminophylline Contraindications
- Associated Side Effects of Aminophylline
- Aminophylline Dosage
- Aminophylline vs Theophylline
- Aminophylline Before and After
- FAQs
- Aminophylline References
Potential Benefits of Aminophylline
Aminophylline offers various health benefits, including weight loss promotion, enhanced cognitive function, improved sleep quality, better cardiovascular health, treatment of lung diseases and injuries, as well as enhanced kidney function.
- Promotes weight loss [1-13]
- Improves cognitive function [14-26]
- Improves sleep quality [27-33]
- Improves cardiovascular health [34-52]
- Treats lung diseases/injuries [53-93]
- Improves kidney function [94-129]
Key Takeaways of Aminophylline
- Aminophylline is commonly used as a bronchodilator to treat respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD). It relaxes the airway muscles, making it easier to breathe.
- Aminophylline therapy requires careful dosing and monitoring of serum theophylline concentrations to maintain therapeutic levels and avoid toxicity. Adjustments to the dose may be necessary based on an individual’s response and potential side effects.
- Aminophylline acts more rapidly than theophylline, making it suitable for situations requiring quick relief from bronchospasms or respiratory distress.
- Like any medication, aminophylline can cause side effects, including nausea, vomiting, nervousness, and cardiac arrhythmias (changes in heart rhythm). Patients should be monitored for adverse reactions during treatment.
- Beyond its role as a bronchodilator, aminophylline may have potential applications in specific medical conditions, such as improving cardiovascular performance in COPD patients or treating central sleep apneas. Always consult with a healthcare professional for accurate dosing and guidance.
What is Aminophylline?
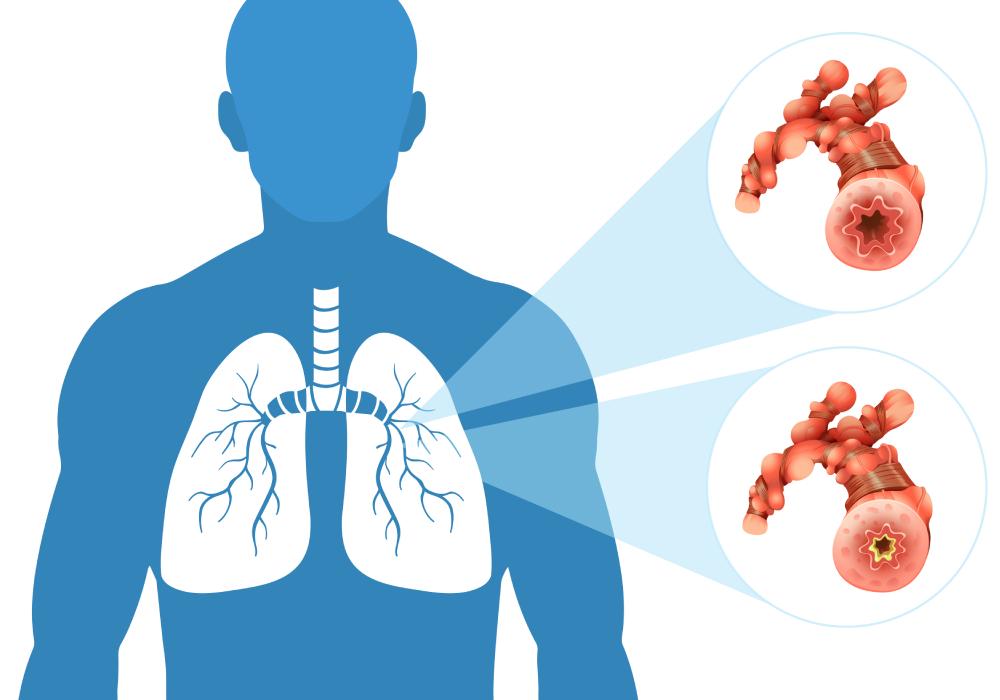
Aminophylline is known as a potent bronchodilator medicine. This means that it opens the airways of the lungs by relaxing the smooth muscles. Because of this effect, aminophylline is prescribed for the treatment of wheezing, breathing difficulties, asthma, emphysema, chronic bronchitis, acute bronchospasm, and other respiratory disorders.
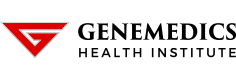
Aminophylline Mechanism of Action
Aminophylline inhibits the enzyme phosphodiesterase-4 (PDE-4) which is found in cells of the lungs. PDE-4 inhibition increases the levels of intracellular cyclic adenosine monophosphate (cAMP) in target cells. This process results in the following effects:
- Relaxation of the smooth muscles of the lungs to allow more air in
- Reduction of inflammation by decreasing the sensitivity of the lungs to allergens
- Increased contractions of the diaphragm
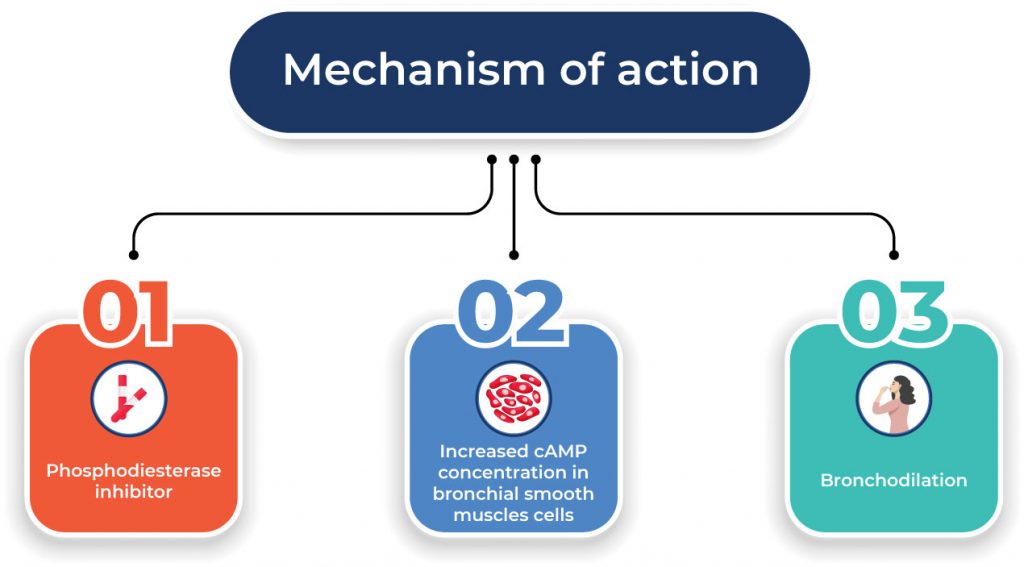
Chemical Structure of Aminophylline
Research on Aminophylline
Promotes Weight Loss
A good deal of evidence suggests that aminophylline can improve body composition by reducing body fat percentage and promoting lean muscle mass:
- In overweight men and women, the application of 0.5% aminophylline cream to the waist twice a day was associated with a significant reduction in waist circumference. [1]
- In participants with fat deposits on their thighs, the application of aminophylline lotion significantly reduced thigh circumference, thigh skinfold thickness, and thigh fat mass. [2]
- Twelve weeks of 0.5% aminophylline cream administration significantly decreased waist-to-hip ratios in overweight female participants compared to male participants. [3]
- A study found that aminophylline promotes fat loss by inducing the breakdown of fat cells. [4]
- In women with lower body fat distribution, the application of aminophylline cream significantly reduced thigh fat. [5]
- In overweight women, the application of 10% aminophylline ointment to the thigh five times a week for 6 weeks with diet and walking resulted in significant girth loss from the treated thigh. [6]
- In sedentary females, the application of a cream containing aminophylline, caffeine, yohimbe, l-carnitine, and gotu kola twice daily for 28 days was more effective at reducing thigh circumference, thigh skinfold thickness, and thigh fat mass compared to a placebo combined with a walking program and a restricted caloric intake. [7]
- In patients with cellulite (persistent subcutaneous fat causing dimpling of the skin), the application of aminophylline cream resulted in fat reduction and improvements in the texture of the skin. [8-10]
- A review of data from two small clinical trials showed that the use of aminophylline cream was associated with reduced thigh girth with no adverse effects. [11]
- In obese women who were placed on a calorie-restricted diet, the application of aminophylline cream resulted in significant girth loss compared with a placebo injection or cream. [12]
In female subjects, the application of aminophylline cream to areas with unwanted body fat for 6 weeks caused a significant reduction in subcutaneous fat and girth. [13]
Improves Cognitive Function

- The administration of escalating doses of aminophylline in patients who received sevoflurane anesthesia accelerated postoperative cognitive recovery. [14-16]
- In school-aged patients, aminophylline administration led to greater improvement on all tests of memory and concentration. [17]
- In patients with brain damage, aminophylline administration improved cognitive function by increasing oxygen levels within the brain. [18]
- In healthy, male, moderate drinkers, treatment with aminophylline (200 mg) significantly reduced ethanol’s effects on the electroencephalogram (EEG) and motor coordination. [19]
- In rats exposed to restrain stress, aminophylline (4mg/kg) modulated the stress in a significant manner. [20]
- In patients anesthetized with total intravenous anesthesia, the administration of aminophylline at 4 mg/kg shortened cognitive recovery time. [21]
- In rats exposed to low oxygen levels, immediate administration of aminophylline significantly improved long-term neurobehavioral achievements. [22]
- In patients who received isoflurane anesthesia, the administration of high doses of aminophylline expedited the extubation (tube removal) time and was associated with improved recovery of vigilance and neuromotor functions. [23-24]
- In patients who received halothane, a general anesthesia, the administration of aminophylline accelerated cognitive recovery. [25]
- In patients who received total intravenous anesthesia (TIVA) with propofol and remifentanil, aminophylline 3 mg/kg shortened the time to spontaneous ventilation and improved early recovery without adverse side effects. [26]
Improves Sleep Quality
Aminophylline administration can also help treat sleeping difficulties associated with various medical conditions:
- In healthy male volunteers, aminophylline administration normalized high-altitude sleep-disordered breathing. [27]
- In patients with obstructive sleep apnea syndrome (a condition in which the walls of the throat interrupt normal breathing during sleep), aminophylline improved impaired breathing and increased NREM (non-rapid eye movement) sleep or dreamless sleep. [28]
- In patients with sleeping difficulties related to acute mountain sickness, aminophylline administration improved sleep efficiency without any adverse effects. [29]
- In a patient with severe, predominantly central sleep apnea (a potentially serious sleep disorder in which breathing repeatedly stops and starts) due to damage to the medulla, the bottom-most part of the brain, aminophylline administration improved respiration at the onset of sleep. [30]
- In thiopental-anesthetized rats, aminophylline improved sleep times and transmission of nerve signals in the brain. [31]
- In mature infants with sleep apnea syndrome, aminophylline treatment for 1 week significantly reduced apneas (breathing repeatedly stops and starts) and cyanosis (bluish skin discoloration) during sleep. [32-33]
Improves Cardiovascular Health
There’s also increasing evidence showing that aminophylline can help improve heart health:
- A study found that aminophylline has the ability to restore normal heart rhythm, thus reducing the risk of heart failure and other fatal heart conditions. [34]
- In chronic obstructive pulmonary disease (COPD) patients, oral and intravenous administration of aminophylline enhanced both right and left heart systolic pump function. [35-36]
- In human subjects, aminophylline administration increased heart rate and cardiac output via stimulation of the sympathetic nervous system. [37-38]
- In COPD patients, aminophylline administration improved global cardiac function and reduced dyspnea (difficulty in breathing). [39-40]
- In animal models, aminophylline improved left ventricular contractility and heart rate variability (interval between heartbeats). [41-42]
- In patients with an occluded heart artery, intravenous aminophylline infusion at 5 mg/kg over 20 minutes significantly delayed the time to onset of exercise-induced ischemia (insufficient blood flow) and improved blood circulation. [43]
- In patients with congenital or acquired heart disease, aminophylline caused a decrease in arterial pressure, left ventricular pressure, right and left atrial pressure, total systemic resistance, and total pulmonary resistance. [44]
- In patients with cardiac failure due to hypertension or coronary heart disease, aminophylline produced consistent and significant increases in cardiac output while decreasing heart pressure. [45]
- In patients with acute inferior myocardial infarction treated with aspirin and streptokinase (a medication that dissolves blood clots), the addition of intravenous aminophylline reversed abnormal heart rhythm. [46]
- In patients with cardiac arrest who do not respond to the standard treatment, the administration of aminophylline (rapid intravenous injection of 250 mg) established a stable heart rhythm with sufficient blood pressure. [47]
- In rabbit hearts, small doses of aminophylline increased the rate and amplitude of heart contractions. [48]
- In patients with angina (chest pain due to reduced blood flow to the heart muscle), a reduction in the total number of episodes of chest pain was reported by the subjects after 6 weeks of aminophylline treatment. [49]
- In patients with severe cases of bradycardia (abnormally low heart rate) who do not respond to the standard treatment, intravenous aminophylline eliminated the need for pacemaker placement. [50]
- In patients with symptomatic bradycardia due to spinal cord injury, the addition of aminophylline to the therapeutic regimen was associated with the resolution of the bradycardia. [51]
- In patients with valvular heart disease, aminophylline increased blood circulation to the heart and lungs by inducing vasodilation (widening of the blood vessels). [52]
Treats Lung Diseases/Injuries
Aminophylline is often prescribed for a multitude of lung conditions. There’s robust evidence supporting the benefits of this drug on pulmonary health:
- In adults hospitalized for acute asthma, treatment with aminophylline was associated with fewer nebulizations of albuterol and a lower rate of exacerbations (worsening of symptoms). [53-54]
- In patients with acute severe asthma, aminophylline infusions improved lung function and symptoms. [55]
- In patients with respiratory fatigue, aminophylline administration reduced the risk of intubation. [56]
- In patients with partially reversible severe airway obstruction, intravenous injection of aminophylline (250 mg) was associated with consistent improvement in the mean forced expiratory volume, a measure of how much air a person can exhale during a forced breath. [57]
- In patients with acute exacerbation of asthma or chronic obstructive pulmonary disease, aminophylline infusion decreased hospital admissions. [58]
- In patients with chronic obstructive pulmonary disease (COPD), aminophylline administration improved symptoms by reducing the levels of inflammatory markers. [59]
- In patients with COPD, oral administration of aminophylline (400 mg) increased mean forced expiratory volume and forced vital capacity. [60-61]
- In patients with COPD, low-dose aminophylline increased the efficacy of inhaled corticosteroids by reducing the incidence of exacerbations. [62-63]
- In patients undergoing valve replacement, aminophylline administration had an anti-inflammatory effect and improved pulmonary oxygenation. [64]
- The prolonged use of maintenance aminophylline therapy in COPD patients increased diaphragmatic contractility and endurance and improved several aspects of mucociliary function (defense mechanism of the lungs). [65]
- The administration of long-acting 225-mg aminophylline compounds twice daily for 8 weeks improved the peak expiratory flow rate in younger COPD patients and relieved symptoms of chest tightness in older COPD patients. [66]
- Aminophylline administration in COPD patients enhanced the anti-inflammatory effect of corticosteroids. [67]
- In patients with chronic bronchitis and moderate to severe chronic obstruction to airflow, aminophylline administration at 800 mg daily led to an improvement in peripheral ventilation. [68]
- In normal young adults, aminophylline prevented alterations in breathing patterns. [69]
- In patients with mild asthma, low-dose aminophylline led to a significant reduction in mean sputum eosinophils (a measure of allergic reaction). [70]
- In patients with atopic asthma, aminophylline administration at 200 mg every 12 hours reduced airway inflammatory response to allergen inhalation. [71]
- In patients with right-sided heart failure due to COPD, aminophylline produced a significant reduction in mean pulmonary artery pressure and increased alveolar ventilation (a process by which oxygen is brought into the lungs). [72]
- In chronic asthmatic patients with regular nocturnal exacerbations who took 450 mg slow-release aminophylline at midnight, a significant increase in mean peak expiratory flow rates (a measure of air flowing out of the lungs) was observed. [73]
- In animal models, aminophylline administration improved survival by enhancing lung maturation. [74-79]
- In animal models of meconium aspiration syndrome, a condition in which a newborn breathes in a mixture of meconium (the earliest stool of an infant) and amniotic fluid into the lungs, aminophylline treatment enhanced lung functions and alleviated oxidative injury and changes in airway reactivity related to lung inflammation. [80-82]
- In mice, the administration of aminophylline (20/kg twice daily) attenuated lung scarring by decreasing collagen production. [83]
- In healthy subjects, aminophylline significantly improved the contractile function of the exhausted human diaphragm, rendering it less susceptible to fatigue. [84-86]
- In rabbits with pulmonary edema (lung inflammation) due to acid injury, aminophylline prevented the increase in lung weight and pulmonary artery pressure. [87-88]
- A study found that high doses of aminophylline may diminish inflammatory recruitment of neutrophils to the lungs, thus reducing injury. [89]
- In children over two years receiving inhaled bronchodilators, aminophylline treatment resulted in greater improvement in lung function compared with placebo. [90]
- A cell study found that aminophylline protected lung cells against programmed cell death (apoptosis) induced by cigarette smoking. [91]
- In premature infants, the administration of aminophylline reduced the risk of chronic lung disease and respiratory distress. [92-93]
Improves Kidney Function
Numerous studies also support the beneficial effects of aminophylline on kidney function and related diseases:
- In patients with acute kidney injury, aminophylline therapy significantly improved renal excretory function as evidenced by increased urine output. [94]
- In neonates and children, a single dose of aminophylline prevented acute kidney injury and severe renal dysfunction. [95]
- In patients with renal colic, a type of pain associated with kidney stones, the administration of 375 mg of aminophylline reduced pain by 24% to 39%. [96]
- Aminophylline administration also reduced the prevalence of acute kidney injury after cardiac surgery in pediatric patients. [97]
- In patients with acute renal failure, aminophylline administration was associated with an improvement in renal function indices. [98]
- In premature infants, aminophylline improved kidney function by enhancing urinary calcium and uric acid excretion. [99]
- Intravenous aminophylline administration in human subjects was associated with a 52% reduction in the risk of contrast-induced acute kidney injury. [100-101]
- In intensive care unit patients with acute kidney injury, aminophylline infusion at 5 mg/kg increased urine output. [102]
- In patients admitted to a general intensive care unit following major surgery, aminophylline administration increased blood flow to the kidneys and improved the glomerular filtration rate (filtering ability of the kidneys). [103]
- In patients undergoing chemotherapy, aminophylline administration prevented the deterioration of the glomerular filtration rate. [104]
- In patients with contrast-induced acute renal failure after coronary angioplasty, the administration of aminophylline countered the harmful effects of the contrast on the kidneys. [105]
- In patients with stones in the urethra, aminophylline reduced stone migration to the kidneys. [106]
- In mice with renal ischemia (insufficient blood flow to the kidneys), aminophylline administration at 5 mg/kg improved renal function and indexes of kidney inflammation. [107]
- In pediatric patients with acute kidney injury, aminophylline administration improved kidney function by increasing urine output and preventing complications. [108-110]
- In pediatric patients who had heart surgery, the administration of aminophylline prevented acute kidney injury and resulted in a significant increase in urine output. [111-116]
- In neonates with low oxygen levels, aminophylline use was associated with an increase in urine output and improvement in the glomerular filtration rate. [117-120]
- In patients who had coronary angiography, a procedure that uses contrast to visualize how blood flows through your heart on an X-ray screen, aminophylline prevented contrast-induced kidney deterioration. [121]
- In patients with liver cirrhosis (liver damage due to scarring), the administration of aminophylline at 3 mg/kg increased free-water production. [122]
- In rats with vancomycin-induced acute kidney injury, the administration of aminophylline at a dose of 24 mg/kg once daily significantly reduced the elevations in kidney enzymes. [123]
- In rats with acute kidney failure caused by the chemotherapeutic drug cisplatin, aminophylline administration at 24 mg/kg every 12 hours alleviated kidney dysfunction. [124]
- In patients with severe chronic kidney disease (CKD), aminophylline significantly reduced the prevalence of gastrointestinal adverse effects associated with traditional treatment for CKD. [125-126]
- In patients with acute kidney injury, aminophylline improved urine flow rate (UFR) and reduced the need for dialysis. [127]
- In high-risk patients, the use of aminophylline infusion was associated with a lower incidence of deterioration in kidney function following heart surgery. [128-129]
Aminophylline Uses
Aminophylline, known by the aminophylline brand name “Phyllocontin” among others, is a bronchodilator that is used to treat and prevent the symptoms of asthma, bronchitis, chronic obstructive pulmonary disease (COPD), and other lung conditions. It’s essential to be aware of different brand names, as they can vary depending on the region or country. Always consult with a healthcare professional when seeking information about specific medications.
The following are aminophylline indications:
Asthma
Aminophylline is used to treat acute exacerbations of asthma and can help prevent asthma attacks by relaxing the muscles around the airways.
COPD (Chronic Obstructive Pulmonary Disease)
Chronic obstructive pulmonary disease, which includes conditions like chronic bronchitis and emphysema, can also be managed with aminophylline. It helps reduce breathlessness and wheezing in these patients.
Bronchitis
This drug helps in alleviating the symptoms of bronchitis by opening the bronchial airways, facilitating better airflow.
Apnea in Premature Infants
Aminophylline can be used to stimulate breathing in premature infants who suffer from apnea (periods when breathing stops).
Diagnostic Testing
Sometimes, aminophylline is used as part of diagnostic tests for certain respiratory conditions, such as asthma and other chronic lung diseases, because of its ability to open up the airways.
Aminophylline works by relaxing and opening air passages in the lungs, making it easier to breathe. The drug is a combination of theophylline and ethylenediamine. It’s essential to monitor theophylline blood levels when using aminophylline, as the therapeutic range is narrow, and there’s a risk of side effects if levels become too high. Always use aminophylline as directed by a healthcare professional to manage conditions like asthma and other chronic lung diseases effectively.
Aminophylline Contraindications
Aminophylline is a medication that is used to treat certain respiratory conditions, such as asthma and chronic obstructive pulmonary disease (COPD). However, there are several contraindications or situations in which aminophylline should not be used. These contraindications include:
Hypersensitivity
Aminophylline should not be used in individuals who have a known hypersensitivity or allergy to aminophylline, theophylline, or other xanthine derivatives.
Active Peptic Ulcer Disease
Aminophylline can increase gastric acid secretion, which may exacerbate symptoms and worsen peptic ulcer disease. It should be avoided in individuals with active peptic ulcers.
Seizure Disorders
Aminophylline can lower the seizure threshold, making seizures more likely to occur. It should be used with caution in individuals with underlying seizure disorders.
Cardiac Arrhythmias
Aminophylline can lead to cardiac arrhythmias, especially in high doses, which may result in an increased risk of severe heart rhythm disturbances. Therefore, it should be avoided or used with extreme caution in individuals with pre-existing arrhythmias, as they may be at an increased risk of experiencing these potentially dangerous side effects.
Congestive Heart Failure
Aminophylline may exacerbate congestive heart failure symptoms. It should be used cautiously, if at all, in individuals with heart failure.
Liver Disease
Individuals with severe liver disease or hepatic dysfunction may have impaired clearance of aminophylline from the body, leading to higher blood levels and an increased risk of toxicity. This is because the liver plays a crucial role in metabolizing and eliminating aminophylline. In cases of hepatic dysfunction, the liver’s ability to perform these metabolic processes may be compromised. As a result, the drug may accumulate in the bloodstream, potentially causing adverse effects such as nausea, vomiting, cardiac arrhythmias, and seizures. Healthcare providers should exercise caution when prescribing aminophylline to individuals with hepatic dysfunction and consider dose reduction or alternative treatments to minimize the risk of toxicity. Regular monitoring of serum theophylline concentrations is essential in such cases to ensure that a safe and effective dose is maintained.
Active Gastrointestinal Bleeding
Aminophylline can irritate the gastrointestinal tract and increase the risk of bleeding. It should not be used in cases of active gastrointestinal bleeding.
Thyroid Disorders
Aminophylline may affect thyroid hormone levels. It should be used with caution in individuals with thyroid disorders.
Children and Elderly
Special caution should be exercised when using aminophylline in children and the elderly, as they may be more sensitive to its effects.
Pregnancy and Breastfeeding
Aminophylline should be used during pregnancy or breastfeeding only if the potential benefits outweigh the risks, and under the supervision of a healthcare provider. It’s essential to discuss your medical history and any pre-existing conditions with your healthcare provider before starting aminophylline or any new medication to ensure it is safe and appropriate for your specific situation. During breastfeeding, aminophylline may pass into breast milk, potentially affecting the nursing infant. Therefore, your healthcare provider should carefully consider the necessity of aminophylline treatment while breastfeeding and monitor both the mother and baby for any adverse effects.
Associated Side Effects of Aminophylline
Aminophylline side effects are very uncommon. There have been some side effects associated with the use of this drug wherein the patient had one of the issues listed below at some point while being on aminophylline. However, these side effects weren’t confirmed to be associated with the treatment and could have been a coincidence and not related to the use of aminophylline. Despite this, it was listed as a side effect associated with aminophylline even though these associated side effects are very uncommon.
Side effects associated with aminophylline may include the following:
- Allergic skin reaction
- Changes in heartbeat and heart rhythm
- Elevated liver enzymes
- Headache
- Heartburn
- Increase in urine volume
- Increased gastric acid secretion
- Insomnia
- Irritability
- Nausea
- Restlessness
- Shakiness
- Vomiting
- Yellow skin and eyes
Aminophylline Dosage
The dosage of aminophylline can vary depending on the specific medical condition being treated, the patient’s age, weight, and overall health, as well as the formulation of the medication (oral, intravenous, etc.). In general, aminophylline dosage in mcg/mL is typically between 10 and 20 mcg/mL. This is the therapeutic range, meaning that this is the range of concentrations that is most likely to be effective in treating asthma and other respiratory conditions without causing side effects. It is crucial to follow the prescribing healthcare provider’s instructions and the dosing information provided on the medication label or packaging. Typically, aminophylline is administered as an injection or oral tablet.
For the treatment of acute bronchospasm in adults, the usual recommended intravenous dosage is an initial loading dose of 5-6 mg/kg of aminophylline infused over 20-30 minutes, followed by a continuous intravenous infusion at a rate of 0.4-0.9 mg/kg/hour to maintain therapeutic levels. The total daily dose should not typically exceed 800 mg unless specifically directed by a healthcare provider. Adjustments in the maintenance dose may be necessary based on the patient’s response to ensure they receive therapeutic doses of the medication.
For children, the dosage may be different and should be determined by a healthcare provider based on the child’s weight and condition. The use of divided doses may be considered to achieve the desired therapeutic effect while minimizing side effects. Dose reduction may also be a consideration if the patient experiences adverse reactions or if serum theophylline concentrations exceed the therapeutic range.
It’s important to note that aminophylline therapy often requires careful monitoring of blood levels (serum theophylline concentrations) to avoid toxicity. Dosing adjustments, including both dose reduction and modification of the maintenance dose, may be necessary based on the patient’s response and any potential side effects. Always consult a healthcare professional or physician for the most accurate and appropriate dosage adjustments for your specific medical situation.
Aminophylline vs Theophylline
Aminophylline and theophylline are both medications that belong to a class of drugs called methylxanthines. While they have some similarities, they also have distinct differences:
Chemical Composition
Aminophylline: Aminophylline is a compound composed of theophylline and ethylenediamine. It is a water-soluble derivative of theophylline.
Theophylline: Theophylline is a naturally occurring compound and is the primary active component of aminophylline. When theophylline is administered intravenously, it can lead to increased serum theophylline levels due to its rapid absorption into the bloodstream. This increased theophylline concentration can be particularly concerning in patients with decreased theophylline clearance, such as those with liver or kidney impairment, as they are at a higher risk of experiencing toxic effects.
Medical Uses
Aminophylline: Aminophylline is typically used in emergency situations and acute care settings, such as in the treatment of severe asthma attacks or chronic obstructive pulmonary disease (COPD) exacerbations. Its administration aims to rapidly achieve therapeutic serum concentrations to address the acute respiratory distress seen in these conditions. Monitoring serum concentrations is essential to ensure appropriate drug dosing and effectiveness during the treatment process.
Theophylline: Theophylline is used for the long-term management and prevention of asthma and COPD symptoms. It is taken regularly to maintain stable respiratory function. Regular monitoring of theophylline clearance is essential in patients receiving theophylline therapy to ensure that serum theophylline levels remain within the therapeutic range. Elevated serum theophylline levels can lead to adverse effects, including nausea, vomiting, cardiac arrhythmias, and seizures. Healthcare providers must adjust theophylline dosage based on the patient’s individual theophylline clearance rate to optimize therapeutic benefits while minimizing the risk of toxicity.
While theophylline itself is not a histone deacetylase activator (a substance that helps control how genes work in our cells by modifying the structure of proteins called histones), it plays a crucial role in managing respiratory conditions by modulating bronchial smooth muscle tone and inflammation, which are essential factors in asthma and COPD management.
It’s important for healthcare professionals to recognize that factors such as age, smoking status, and concurrent medication use can also influence theophylline clearance. Therefore, individualized dosing and vigilant monitoring of serum theophylline levels are crucial to providing safe and effective theophylline therapy for patients with respiratory conditions like asthma or chronic obstructive pulmonary disease (COPD).
Administration
Aminophylline: Aminophylline injection is often administered intravenously (IV) or intramuscularly (IM) in acute situations where a rapid response is needed. Serum concentrations of aminophylline injection are closely monitored during administration to ensure the desired therapeutic effect and to prevent adverse reactions. It is essential for healthcare providers to maintain appropriate serum concentrations of aminophylline injection to achieve the desired clinical outcomes. Proper monitoring of aminophylline injection levels allows healthcare professionals to adjust the dose as needed for optimal patient care.
Theophylline: Serum theophylline concentrations are usually monitored closely in patients taking theophylline to ensure its therapeutic levels are maintained. Theophylline is usually taken orally in the form of tablets, capsules, or extended-release preparations. It is designed for chronic use and provides a sustained effect. Serum theophylline concentrations are usually monitored closely in patients taking theophylline to ensure its therapeutic levels are maintained.
Onset of Action
Aminophylline: Aminophylline acts more rapidly than theophylline, making it suitable for situations requiring quick relief, such as acute bronchospasms. This rapid onset of action is due to the fact that aminophylline injection rapidly undergoes metabolic conversion within the body, leading to the release of theophylline, which then exerts its bronchodilatory effects. Understanding theophylline metabolism is essential in this context, as the conversion of aminophylline injection to theophylline increases its bioavailability and therapeutic efficacy. Theophylline metabolism is influenced by factors such as liver function, age, genetics, and drug interactions, which can affect the rate at which aminophylline injection is converted to the active theophylline compound. Therefore, healthcare providers must consider these factors when determining the appropriate use of aminophylline injection in clinical practice.
Theophylline: Theophylline has a slower onset of action and is used for maintenance therapy to prevent respiratory symptoms over an extended period. Monitoring serum theophylline concentrations is essential to ensure therapeutic efficacy and prevent toxicity. Regular assessment of serum theophylline concentration allows healthcare providers to adjust dosage regimens as needed, ensuring that patients maintain optimal drug levels for effective management of their respiratory conditions. Additionally, healthcare professionals can use serum theophylline concentration measurements to identify and address any potential signs of theophylline overdose or toxicity in a timely manner, promoting patient safety during the course of treatment.
It’s important to note that theophylline distributes poorly into tissues with high-fat content, which can affect its pharmacokinetics. Factors such as age, liver function, and concurrent use of other medications can also influence theophylline clearance. Healthcare providers may consider dose adjustments or therapeutic drug monitoring to increase theophylline clearance in patients with altered pharmacokinetics. Utilizing anhydrous theophylline formulations can also play a role in maintaining consistent drug levels and optimizing therapeutic outcomes, as these formulations offer precise dosing options and can contribute to better control of serum theophylline concentration.
Half-Life
Aminophylline: Aminophylline has a shorter half-life compared to theophylline. The difference in half-life can be attributed to the fact that aminophylline injection consists of theophylline and ethylenediamine, which is rapidly converted into theophylline in the body. This conversion process contributes to the faster onset of action and shorter duration of effect observed with aminophylline injection.
It’s important to note that aminophylline clearance is influenced by various factors, including genetics, liver function, and drug interactions. Additionally, theophylline administered to individuals with certain medical conditions may result in altered metabolism rates. Understanding these nuances in theophylline metabolism is crucial for healthcare providers to optimize drug therapy and minimize the risk of adverse effects.
Theophylline: Serum theophylline concentrations are routinely monitored in patients receiving theophylline therapy to ensure therapeutic levels are maintained. Theophylline clearance varies among individuals, and regular monitoring of serum theophylline concentrations helps healthcare providers adjust dosage regimens to achieve optimal therapeutic levels while minimizing the risk of toxicity. This careful management of serum theophylline concentrations is essential for the safe and effective treatment of conditions such as asthma or chronic obstructive pulmonary disease (COPD).
Theophylline metabolism can be influenced by various factors, including age, liver function, and concurrent medications. Healthcare providers need to be vigilant in monitoring serum theophylline concentrations and theophylline metabolism in patients with these considerations. It’s crucial to assess how theophylline is being metabolized in an individual patient and whether the dosage regimen needs modification.
In some cases, anhydrous theophylline formulations may be preferred, as they offer precise dosing options and can contribute to better control of serum theophylline concentrations. These formulations can be particularly beneficial when fine-tuning theophylline therapy in patients with varying clearance rates. By closely monitoring theophylline clearance and utilizing appropriate formulations, healthcare providers can optimize treatment outcomes while ensuring patient safety.
Dosage Monitoring
Aminophylline: Aminophylline levels, specifically serum concentrations, are usually monitored closely in emergency situations to avoid toxicity. Regular monitoring of serum concentrations ensures that aminophylline clearance remains within the therapeutic range (commonly measured in mcg/ml) and helps prevent adverse effects. Healthcare providers use these serum concentration measurements to make informed decisions about dosage adjustment or the need for additional interventions to maintain aminophylline levels within safe and effective limits, typically within the recommended therapeutic range. Monitoring also allows healthcare professionals to tailor the treatment to the patient’s specific needs, ensuring the best possible outcome in emergency situations where aminophylline is administered.
Theophylline: Serum theophylline concentrations are monitored regularly in chronic therapy to ensure that therapeutic levels are maintained and to prevent toxicity. Monitoring serum theophylline concentrations, which reflect theophylline clearance, is crucial for adjusting dosage regimens and optimizing the management of individuals receiving theophylline therapy. It allows healthcare providers to fine-tune treatment to achieve the desired therapeutic effect while avoiding potentially harmful levels of the drug in the bloodstream.
Additionally, healthcare providers use serum theophylline concentrations, a key indicator of theophylline clearance, to make informed decisions regarding dose adjustments and to minimize the risk of adverse effects associated with theophylline therapy. Monitoring theophylline clearance is an essential part of ensuring the safe and effective use of this medication. Your healthcare provider will adjust dose as per clinical needs.
Side Effects and Safety
Both aminophylline and theophylline can have side effects, including nausea, vomiting, nervousness, and cardiac arrhythmias. However, aminophylline may have a higher risk of adverse effects due to its more rapid action. Additionally, monitoring serum concentrations of both drugs is essential to ensure that they remain within the therapeutic range and do not lead to toxic effects.
The term “narrow therapeutic index” refers to medications that have a small margin of safety between their minimum effective dose and the minimum toxic dose. In other words, drugs with a narrow therapeutic index have a small window between the dose that provides a therapeutic effect and the dose that can lead to harmful or toxic effects. For such medications, it is crucial to maintain drug levels within this narrow range to achieve the desired therapeutic outcome while avoiding harmful side effects.
In the context of aminophylline and theophylline, both drugs fall under the category of medications with a narrow therapeutic index. This means that maintaining the serum concentrations of these drugs within a specific range is essential to ensure their effectiveness and safety. Deviating from this narrow range can lead to adverse effects, including nausea, vomiting, nervousness, and cardiac arrhythmias. Aminophylline, in particular, carries a higher risk of adverse effects due to its more rapid action.
Therefore, it is imperative for healthcare providers to regularly monitor serum theophylline concentrations when prescribing these drugs. By doing so, they can make informed decisions about dose adjustments, if necessary, to keep the drug levels within the therapeutic range. This monitoring helps optimize the therapeutic benefits of aminophylline and theophylline while minimizing the potential for toxic effects, ensuring the safe and effective management of various medical conditions.
Regularly assessing serum theophylline concentration is also crucial to maintaining optimal drug levels and minimizing the risk of side effects. Healthcare providers should closely monitor these levels to make necessary adjustments in the treatment regimen if needed, ensuring the safety and effectiveness of theophylline therapy.
Availability
Aminophylline: Aminophylline is typically administered in healthcare settings by healthcare professionals. The dosage and administration of aminophylline are carefully monitored to maintain appropriate serum concentrations within the therapeutic range, typically measured in mcg/ml, ensuring the desired clinical effects while minimizing the risk of adverse reactions. This close monitoring of serum concentrations helps healthcare providers make informed decisions regarding dosage adjustments and the overall management of aminophylline therapy for the patient’s specific medical condition.
Theophylline: Theophylline is available in various oral formulations and is prescribed for home use under medical supervision. However, in certain clinical situations where rapid onset of action is required, intravenous theophylline may be administered. It’s important to note that the rate of absorption and onset of action of intravenous theophylline differs significantly from oral theophylline.
When theophylline is administered intravenously, it undergoes rapid absorption into the bloodstream, leading to an immediate increase in serum theophylline levels. This rapid increase can be advantageous in situations where prompt therapeutic effects are needed, such as in the management of acute exacerbations of respiratory conditions like asthma.
On the other hand, oral theophylline typically has a slower onset of action, as it must first be absorbed from the gastrointestinal tract before entering the bloodstream. While it can provide long-term maintenance therapy for chronic respiratory conditions, it may not be suitable for rapidly addressing acute symptoms.
Healthcare providers must carefully consider the appropriate route of administration and dosage when prescribing theophylline to patients based on their clinical presentation and treatment goals. Close monitoring of theophylline levels is crucial, as both intravenous and oral theophylline increases carry the potential for adverse effects if serum concentrations exceed the therapeutic range.
In summary, while aminophylline and theophylline are related medications with similar therapeutic effects, they are used in different clinical scenarios and have variations in administration, onset of action, and safety profiles. The choice between them depends on the specific medical condition and the required treatment approach. Patients should always follow their healthcare provider’s recommendations regarding the use of these medications.
Aminophylline Before and After
About Dr. George Shanlikian
Dr. George Shanlikian, renowned as the world’s best hormone therapy doctor, possesses expertise in various medical domains. These include Bio-Identical Hormone Replacement Therapy, Peptide Replacement Therapy, Anti-Aging Medicine, Regenerative Medicine, Stress Management, Nutrition Consulting, Nutritional Supplement Consulting, and Exercise Consulting.
Read more about him here: https://www.genemedics.com/dr-george-shanlikian-md-best-hormone-therapy-doctor
Read more success stories here:
Men’s Success Stories: https://www.genemedics.com/about-ghi/ghi-success-stories/mens-success-stories/
Women’s Success Stories: https://www.genemedics.com/about-ghi/ghi-success-stories/womens-success-stories/
FAQ
What should I check before giving aminophylline?
Before giving aminophylline, you should check the patient’s medical history, including any history of hypersensitivity to the drug, pre-existing medical conditions such as heart or liver disease, current medications, and drug interactions. Additionally, it’s essential to assess the potential transfer of aminophylline into breast milk if the patient is a breastfeeding mother, as this could impact a nursing infant. Patients with a history of acute hepatitis should be closely monitored when prescribed aminophylline, as liver function may be compromised, potentially affecting drug metabolism and clearance. It’s essential to consider these factors to ensure the safe and effective administration of aminophylline in clinical practice.
What are the precautions for aminophylline?
Precautions for aminophylline include monitoring for signs of toxicity, especially in patients with a history of aminophylline sensitivity or underlying medical conditions. Aminophylline should be used with caution in patients with heart arrhythmias, seizures, hyperthyroidism, and gastrointestinal disorders, as these conditions may increase the risk of adverse effects, given its narrow therapeutic index.
Careful monitoring of serum theophylline levels is essential to prevent overdose and maintain aminophylline within the appropriate therapeutic range, considering its narrow therapeutic index. Patients with hepatic impairment may metabolize aminophylline differently, potentially leading to altered drug levels, so close monitoring is essential. Additionally, aminophylline can affect renal function, and patients with renal impairment should be closely monitored for any signs of metabolic acidosis or changes in renal function. Irregular heartbeat is a potential side effect of aminophylline, and healthcare providers should closely monitor cardiac function during treatment to detect any signs of irregular heartbeat and take appropriate measures if needed.
For breastfeeding mothers, it’s important to note that aminophylline can pass into breast milk, potentially affecting nursing infants. Healthcare providers should carefully weigh the benefits of aminophylline treatment against the potential risks to the infant, and mothers may need to consider alternative feeding options while undergoing aminophylline therapy. Similarly, pregnant individuals should discuss the potential risks and benefits of aminophylline treatment with their healthcare provider, as the drug may affect the developing fetus.
How often to take aminophylline?
The frequency of aminophylline administration depends on the specific medical condition being treated and the healthcare provider’s prescription. It can be administered as a single dose, multiple doses per day, or as an intravenous infusion. For chronic lung conditions like asthma or chronic obstructive pulmonary disease (COPD), aminophylline is often prescribed as a maintenance therapy, typically with multiple doses per day to ensure a sustained bronchodilatory effect and improved respiratory function.
Dosage adjustment may be necessary based on the patient’s response to treatment and any potential side effects, ensuring that the therapy remains effective and safe over time. Monitoring of serum aminophylline levels, typically measured in mcg/ml, is important in maintaining therapeutic concentrations and avoiding toxicity. Healthcare providers use these measurements to make informed decisions about dosing regimens and to ensure that patients receive the appropriate amount of aminophylline for their specific medical conditions.
When is the best time to take aminophylline?
The timing of aminophylline administration can vary depending on the condition. It is best to follow the healthcare provider’s instructions for the specific dosing schedule. Monitoring the timing of aminophylline administration is crucial to ensure that peak serum concentrations are achieved when needed for the desired therapeutic effect. This timing may be especially important in acute situations where rapid bronchodilation or relief from respiratory distress is required, as achieving peak serum concentrations promptly can help maximize the drug’s effectiveness.
Aminophylline is available in various forms, including oral tablets and an oral solution. The choice of formulation may also influence the timing of administration, as oral solutions may be absorbed more rapidly than tablets, potentially leading to a faster onset of action.
Can aminophylline be taken without food?
Aminophylline is available in various forms, including oral tablets, intravenous injections, and oral solutions. When administering the oral solution, patients should follow the prescribed dosing schedule for consistency. Monitoring the serum concentration of aminophylline is crucial to determine if adjustments in dosage are needed to achieve therapeutic levels and avoid toxicity. This close monitoring helps healthcare providers make informed decisions about the medication’s effectiveness and safety for the patient, regardless of the formulation used.
Why should aminophylline be given slowly?
Aminophylline should be given slowly to minimize the risk of adverse effects and toxicity, particularly in patients with renal impairment, as their ability to clear the drug from the body may be compromised. Rapid administration can lead to serious side effects and should be avoided. Monitoring serum concentration levels is essential during the administration of aminophylline to ensure that the drug remains within the therapeutic range and to prevent any potential complications. Healthcare providers use these serum concentration measurements, typically expressed in mcg/ml, to make informed decisions about dosage adjustments or the need for additional interventions to maintain aminophylline levels within safe and effective limits. Proper dosing and monitoring are crucial to achieving the desired therapeutic outcomes while minimizing the risk of adverse reactions.
Does aminophylline need to be protected from light?
Yes, aminophylline should be protected from light to prevent degradation of the drug. Exposure to light can lead to chemical changes in aminophylline, which may affect its stability and efficacy. It’s essential to store aminophylline in a container that shields it from direct light to maintain the desired serum concentration and therapeutic effects. Proper storage conditions help ensure that the medication remains effective and safe for use. Always follow the recommended storage instructions provided with the specific formulation of aminophylline you are using to maintain its serum concentration within the therapeutic range.
What drugs should not be taken with aminophylline?
Several drugs should not be administered concomitantly with aminophylline, including other xanthine derivatives (xanthine drugs) like theophylline or caffeine, as these substances can potentially impact the central nervous system and serum concentrations of aminophylline, leading to a range of adverse effects. The consideration of potential drug interactions is crucial when prescribing or using aminophylline, as taking it with certain medications can result in a harmful drug combination, affecting its therapeutic effects and safety profile. Healthcare providers must carefully evaluate a patient’s medication regimen to minimize the risk of adverse reactions and ensure the most effective treatment.
To safeguard patient health, it is imperative to provide a comprehensive list of all medications, including vitamin supplements, in use to the healthcare provider. This enables the assessment of potential drug interactions, ensuring that serum concentrations of aminophylline remain within the therapeutic range, thereby promoting safe and effective treatment. Monitoring serum concentration levels is a crucial step in managing these interactions and optimizing patient care, especially considering the potential impact on the central nervous system.
How does aminophylline affect heart rate?
Aminophylline may affect heart rate by increasing it in some cases, especially when administered rapidly, and this effect can be more pronounced in elderly patients due to age-related changes in cardiac function. Such patients may experience a more significant heart rate increase when given aminophylline. Monitoring heart rate is essential during aminophylline therapy in elderly patients to ensure their safety and adjust the dosage if necessary. Additionally, healthcare providers should consider the overall health and medical history of such patients when determining the appropriate use of aminophylline to minimize potential cardiac-related side effects, especially if they have a history of cardiac disease.
What are the desired effects of aminophylline?
The desired effects of aminophylline include bronchodilation, improved airflow, increased oxygen exchange, and relief from symptoms of respiratory distress, such as wheezing and shortness of breath. Aminophylline is commonly used in the management of chronic lung diseases, where it helps alleviate symptoms and improve lung function. Its bronchodilatory properties make it particularly beneficial for individuals with conditions like asthma and chronic obstructive pulmonary disease (COPD). Aminophylline achieves these effects by relaxing the smooth muscle cells lining the airways, reducing constriction, and allowing for easier airflow.
By relaxing airway smooth muscles, aminophylline facilitates easier breathing and enhances overall respiratory function in patients with chronic lung diseases. However, it’s important to note that aminophylline has a narrow therapeutic index, meaning that the difference between a therapeutic dose and a potentially toxic dose is small. Therefore, careful monitoring of serum theophylline concentrations is essential to ensure that patients remain within the safe and effective therapeutic range, minimizing the risk of adverse effects.
Does aminophylline increase respiratory rate?
Aminophylline may increase respiratory rate in some cases, primarily by improving bronchial airflow and oxygenation.
Does aminophylline affect sleep?
Aminophylline can affect sleep in some individuals, potentially causing insomnia or restlessness as a side effect.
Can aminophylline cause tachycardia?
Aminophylline can cause tachycardia (increased heart rate) as a side effect, especially when administered rapidly. This cardiac stimulation is often observed due to aminophylline’s bronchodilatory effects and its impact on adenosine receptors, which can increase heart rate. It is essential for healthcare providers to monitor patients closely when administering aminophylline to detect and manage any cardiovascular side effects promptly. Adjustments to the dosage or infusion rate may be necessary to mitigate the risk of excessive cardiac stimulation and maintain patient safety during treatment.
Does aminophylline cause bradycardia?
Aminophylline is not typically associated with bradycardia (slow heart rate) as a side effect.
Can salbutamol and aminophylline be taken together?
Salbutamol and aminophylline can be taken together in some cases, but the combination should be carefully monitored and prescribed by a healthcare provider. Combining these medications may help achieve better bronchodilation and improved respiratory function in individuals with severe asthma or other respiratory conditions. However, it’s essential to be aware of potential adverse reactions that can arise when using both medications concurrently.
Regular check-ups and close supervision by a healthcare provider are crucial to assess the effectiveness of the combination therapy while minimizing the risk of adverse reactions. Adjustments to the dosages may be necessary based on the patient’s response and the presence of any side effects associated with the combined use of salbutamol and aminophylline.
How does aminophylline help respiratory distress syndrome?
Aminophylline can help treat respiratory distress syndrome by improving bronchial airflow and oxygenation and reducing symptoms of airway constriction, thereby preventing respiratory failure. Monitoring for higher serum concentrations of aminophylline is essential during treatment to ensure that therapeutic levels are maintained and potential side effects are minimized. This careful monitoring plays a critical role in managing respiratory distress syndrome and optimizing patient outcomes.
Is aminophylline used in heart failure?
Aminophylline may be used in heart failure cases under specific circumstances, but it should be prescribed and monitored by a healthcare provider to minimize the risk of cardiovascular complications.
Can aminophylline be given with normal saline?
Aminophylline can be given with normal saline, depending on the patient’s condition and the healthcare provider’s recommendations.
How long to continue aminophylline infusion?
The duration of aminophylline infusion varies based on the patient’s condition and the healthcare provider’s prescription.
How long does aminophylline stay in your system?
Aminophylline can stay in the system for several hours to days, with the exact duration varying among individuals.
Can aminophylline be inhaled?
Aminophylline can be administered via inhalation in some cases, typically using a nebulizer, to treat specific respiratory conditions.
Why is aminophylline important in pulmonary edema?
Aminophylline is important in pulmonary edema because it helps improve bronchial airflow and oxygenation, which can be critical in managing the condition.
What effects does aminophylline have on potassium?
Aminophylline can affect potassium levels in the body, potentially leading to hypokalemia (low potassium levels) as a side effect.
How does aminophylline prevent apnea?
Aminophylline can help prevent apnea in premature infants by stimulating respiratory drive and improving lung function.
Is aminophylline a diuretic?
Aminophylline is not typically considered a diuretic, as its primary function is to improve bronchial function and respiratory symptoms.
What is the use of aminophylline in cardiac?
Aminophylline may be used in cardiac cases to improve bronchial airflow and oxygenation, especially in cases where respiratory distress is a concern.
Does aminophylline cause hyperglycemia?
Aminophylline can sometimes cause hyperglycemia (high blood sugar) as a side effect.
Can aminophylline be used with a nebulizer?
Aminophylline can be used with a nebulizer in specific respiratory conditions, but the administration method should be determined by a healthcare provider.
Which is better aminophylline or salbutamol?
The choice between aminophylline and salbutamol depends on the specific medical condition and the healthcare provider’s prescription.
How does aminophylline affect the kidneys?
Aminophylline may affect kidney function in some cases, potentially leading to changes in urine output. Monitoring kidney function is important during aminophylline therapy to detect any abnormalities or signs of serious toxicity related to kidney function. This monitoring involves regular assessments of urine output, renal function tests, and overall renal health. Healthcare providers closely watch for any signs of kidney dysfunction, such as decreased urine output, elevated creatinine levels, or changes in electrolyte balance, to ensure the safe and effective use of aminophylline in patients.
How does aminophylline affect urine output?
Aminophylline can affect urine output, and changes in urine output should be monitored during treatment.
Can I take Ventolin and aminophylline together?
Ventolin and aminophylline can be taken together in some cases, but the combination should be prescribed and monitored by a healthcare provider.
How do you give aminophylline for asthma?
The administration of aminophylline for asthma varies depending on the specific asthma management plan and should be prescribed and monitored by a healthcare provider. The recommended dosage of aminophylline is typically based on the patient’s weight and is often expressed in micrograms per milliliter (mcg/ml) to ensure precise dosing. It’s crucial for healthcare providers to calculate the appropriate dosage and monitor serum concentrations of aminophylline (mcg/ml) regularly to maintain therapeutic levels and prevent potential side effects or toxicity. This personalized approach helps ensure that patients receive the most effective and safe treatment for their asthma.
Reference
Caruso MK, Pekarovic S, Raum WJ, Greenway F. Topical fat reduction from the waist. Diabetes ObesMetab. 2007;9(3):300-3.
Topical fat reduction from the waist
This study aimed to investigate whether applying aminophylline cream to the waist would reduce waist circumference compared to a control group. Fifty participants with a BMI greater than 27 kg/m(2) were randomized into two groups, with one applying the cream twice daily and the other receiving no treatment to the waist. After 12 weeks, both groups experienced a significant reduction in BMI, with the aminophylline cream group showing a substantial decrease in waist circumference (11 cm) compared to the control group (5 cm). This effect was observed in both men and women, with women achieving greater waist girth loss. The waist to hip ratio, a measure of fat distribution, also improved. Aminophylline levels remained undetectable, and there were no adverse events, suggesting that aminophylline cream is a safe and effective method for localized waist fat reduction.
You can read the abstract of the article at https://dom-pubs.onlinelibrary.wiley.com/doi/10.1111/j.1463-1326.2006.00600.x.
Escalante G, Bryan P, Rodriguez J. Effects of a topical lotion containing aminophylline, caffeine, yohimbe, l-carnitine, and gotu kola on thigh circumference, skinfold thickness, and fat mass in sedentary females. J Cosmet Dermatol. 2018.
Effects of a topical lotion containing aminophylline, caffeine, yohimbe, l-carnitine, and gotu kola on thigh circumference, skinfold thickness, and fat mass in sedentary females
This double-blind, placebo-controlled study examined the impact of Lipoxyderm™, a topical lotion containing aminophylline, caffeine, yohimbe, l-carnitine, and gotu kola, on thigh fat reduction. Seven participants followed a calorie-restricted diet and a 150-minute weekly walking program while applying either Lipoxyderm™ or a placebo to one leg for 28 days. The results showed that Lipoxyderm™, in combination with diet and exercise, led to a significant reduction in thigh circumference (1.2 vs 0.8 cm), skinfold thickness (3.7 vs 2.0 mm), and thigh fat mass (100.0 g vs 57.3 g) compared to the placebo-treated leg, highlighting its potential for enhancing thigh fat loss.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7379994/
Lundberg GD. Fat reduction by topical waist applications may actually work. Medscape J Med. 2008;10(2):43. Published 2008 Feb 21.
Available from https://academic.oup.com/asj/article/17/5/304/177651.
Prospective and Randomized Determination of the Efficacy of Topical Lipolytic Agents
Many manufacturers promote topical creams as a quick solution for eliminating unwanted fat or cellulite, often containing theophylline as their active ingredient. These creams claim to induce lipolysis by binding to adipocyte β-adrenergic receptors and are applied with massage. However, this prospective randomized study involving eleven women of normal body weight who applied either Skinny Dip™ or a placebo for 8 weeks found no statistically significant differences in appearance, abdominal or thigh circumference, or skinfold measurements between the active agent (Skinny Dip™) and the placebo. This study did not provide scientific evidence supporting the effectiveness of topically applied lipolytic creams for eliminating localized fat or cellulite.
You can read the full article at https://academic.oup.com/asj/article/17/5/304/177651.
Available from https://journals.lww.com/plasreconsurg/fulltext/2013/09000/Thigh_Girth_Loss_in_Women_with_Lower_Body_Fat.61.aspx.
Thigh Girth Loss in Women with Lower Body Fat Distribution Increases Breast Volume
In our study, twelve healthy women with a lower body fat distribution applied a 1.5% aminophylline cream to both thighs twice a day for 12 weeks. We aimed to investigate changes in fat distribution in areas not treated with the cream. The results showed that thigh girth decreased by 1.3 cm (p = 0.05), while breast volume increased by 8.9 cc (p < 0.01), indicating a redistribution of body fat from the thighs to the breasts. This unique fat redistribution following local fat reduction with a topical aminophylline-containing lipolytic cream had not been previously reported. Such redistribution may benefit women with lower body fat distribution, helping them achieve their cosmetic goals of smaller thighs and larger breasts during weight loss.
You can read the full article at https://journals.lww.com/plasreconsurg/fulltext/2013/09000/Thigh_Girth_Loss_in_Women_with_Lower_Body_Fat.61.aspx.
Greenway, F. L., Bray, G. A., & Heber, D. (1995). Topical fat reduction. Obesity research, 3 Suppl 4, 561S–568S. https://doi.org/10.1002/j.1550-8528.1995.tb00228.x.
Topical fat reduction
Women often find it challenging to reduce fat in their thigh area, primarily due to heightened alpha-2 adrenergic receptor activity influenced by estrogen. To address this concern, a series of clinical trials was conducted, employing various methods to target thigh fat loss. These trials included injections of isoproterenol, ointments containing forskolin, yohimbine, and aminophylline, and the application of aminophylline cream to the thigh, combined with dietary changes and physical activity. Notably, all trials, except the one involving yohimbine ointment, resulted in significant reductions in thigh girth, suggesting that topical fat reduction for women’s thighs can be achieved effectively without the need for diet or exercise.
You can read the abstract of the article at https://onlinelibrary.wiley.com/doi/abs/10.1002/j.1550-8528.1995.tb00228.x?sid=nlm%3Apubmed.
Escalante, G., Bryan, P., & Rodriguez, J. (2019). Effects of a topical lotion containing aminophylline, caffeine, yohimbe, l-carnitine, and gotu kola on thigh circumference, skinfold thickness, and fat mass in sedentary females. Journal of cosmetic dermatology, 18(4), 1037–1043. https://doi.org/10.1111/jocd.12801.
Effects of a topical lotion containing aminophylline, caffeine, yohimbe, l-carnitine, and gotu kola on thigh circumference, skinfold thickness, and fat mass in sedentary females
This double-blind, placebo-controlled within-group study examined the effects of Lipoxyderm™, containing aminophylline, caffeine, yohimbe, l-carnitine, and gotu kola, on thigh fat loss in conjunction with a low-intensity exercise program and restricted calorie intake. Seven participants underwent pre/post-exercise testing, followed a hypocaloric diet, and were randomly assigned to apply Lipoxyderm™ or a placebo to their legs for 28 days. The study found a significant interaction between time and group for thigh circumference, skinfold thickness, and fat mass, concluding that a twice-daily application of Lipoxyderm™, combined with diet and exercise, was more effective at reducing thigh circumference, skinfold thickness, and thigh fat mass compared to a placebo.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7379994/.
Caruso, M. K., Roberts, A. T., Bissoon, L., Self, K. S., Guillot, T. S., & Greenway, F. L. (2008). An evaluation of mesotherapy solutions for inducing lipolysis and treating cellulite. Journal of plastic, reconstructive & aesthetic surgery : JPRAS, 61(11), 1321–1324. https://doi.org/10.1016/j.bjps.2007.03.039.
An evaluation of mesotherapy solutions for inducing lipolysis and treating cellulite
The study aimed to assess the lipolytic potential of cosmetic mesotherapy solutions commonly used for fat reduction and cellulite treatment. Human fat cell assays were conducted to measure glycerol generation as an indicator of lipolysis. Various mesotherapy solutions were tested, including aminophylline, yohimbine, isoproterenol, melilotus, and combinations of these substances. The results showed that isoproterenol, aminophylline, and yohimbine independently stimulated lipolysis. Additionally, the combination of certain stimulators enhanced lipolysis. Lidocaine was found to inhibit lipolysis, suggesting it should be excluded from mesotherapy solutions intended for localized fat reduction.
You can read the abstract of the article at https://www.jprasurg.com/article/S1748-6815(07)00443-3/fulltext.
Dickinson, B. I., & Gora-Harper, M. L. (1996). Aminophylline for cellulite removal. The Annals of pharmacotherapy, 30(3), 292–293. https://doi.org/10.1177/106002809603000315.
Aminophylline for cellulite removal
The available data on the safety and effectiveness of aminophylline thigh cream are constrained by small study populations and incomplete method disclosure. Although the studies exhibit sound design and promising initial results, further data are required to definitively establish the safety and efficacy of aminophylline thigh cream. Until more comprehensive data becomes accessible, aminophylline thigh cream that has been scientifically validated as both safe and effective remains, as termed by the Washington Post, a “dream cream.”
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/8833567/.
Available from https://journals.sagepub.com/doi/abs/10.1177/229255039500300409.
Available from https://journals.sagepub.com/doi/abs/10.1177/875512259701300209.
Greenway, F. L., & Bray, G. A. (1987). Regional fat loss from the thigh in obese women after adrenergic modulation. Clinical therapeutics, 9(6), 663–669.
Regional fat loss from the thigh in obese women after adrenergic modulation
By applying treatments that either involved isoproterenol injections or creams containing colforsin (forskolin), aminophylline, and yohimbine, along with yohimbine cream, colforsin cream, or aminophylline cream to one thigh of twenty-eight obese women undergoing a calorie-restricted diet for four weeks, a notable reduction in thigh girth was observed in the treated thighs compared to the placebos applied to the opposite thigh, with no reported adverse effects from either the cream or the injections. Consequently, it is inferred that localized fat reduction from the thigh can be safely achieved using these approaches.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/2894247/.
Available from http://www.jarcet.com/articles/Vol14Iss1/Petrofsky3.pdf.
Turan, A., Memiş, D., Karamanlioglu, B., Colak, A., Pamukçu, Z., & Turan, N. (2002). Effect of aminophylline on recovery from sevoflurane anaesthesia. European journal of anaesthesiology, 19(6), 452–454.
Effect of aminophylline on recovery from sevoflurane anaesthesia
In a randomized, double-blind study involving 100 ASA I-II patients scheduled for elective surgery, the effect of aminophylline on recovery from sevoflurane anesthesia was investigated. Patients were divided into two groups, one receiving NaCl 0.9% and the other aminophylline 5mg kg(-1). Both groups were premedicated with atropine and midazolam, and anesthesia was induced with propofol, followed by sevoflurane maintenance. Aminophylline or saline was administered after discontinuation of sevoflurane. While there were no significant differences in mean arterial pressure, peripheral oxygen saturation, or anesthesia duration, heart rate increased significantly after aminophylline, and recovery times, including eye opening, verbal response, extubation, and successful performance of calculations, were significantly shorter in the aminophylline group. This suggests that aminophylline can expedite recovery after sevoflurane anesthesia, potentially offering advantages in clinical practice for patients.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/12094921/.
El tahan MR. Effects of aminophylline on cognitive recovery after sevoflurane anesthesia. J Anesth. 2011;25(5):648-56.
Effects of aminophylline on cognitive recovery after sevoflurane anesthesia
In a study aiming to assess the effects of increasing doses of aminophylline on cognitive and clinical recovery after sevoflurane anesthesia, 150 patients undergoing elective surgery with sevoflurane-fentanyl anesthesia were randomly assigned to receive saline or escalating doses of 2, 3, 4, or 5 mg/kg of aminophylline. Patients who received aminophylline exhibited higher Short Orientation Memory Concentration Test (SOMCT) scores, elevated entropy values for the initial 10 minutes, reduced end-tidal sevoflurane concentrations (EtSevo) during the first 4 minutes after anesthesia, shorter times to eyes opening and extubation, and improved respiratory parameters compared to the placebo group. Particularly, patients receiving 4 and 5 mg/kg of aminophylline showed the greatest cognitive improvement, shorter times to recovery milestones, and faster discharge times, indicating that aminophylline administration can expedite cognitive recovery from sevoflurane anesthesia through enhanced sevoflurane elimination via ventilation.
You can read the abstract of the article at https://link.springer.com/article/10.1007/s00540-011-1190-8.
Turan, A., Memiş, D., Karamanlýodthlu, B., Pamukçu, Z., & Süt, N. (2004). Effect of aminophylline on bispectral index. Acta anaesthesiologica Scandinavica, 48(4), 408–411. https://doi.org/10.1111/j.0001-5172.2004.00350.x.
Effect of aminophylline on bispectral index
In this study, the effects of aminophylline on patients undergoing sevoflurane anesthesia were investigated. Sixty patients scheduled for elective surgery were included, and anesthesia was maintained using sevoflurane to target specific Bispectral Index (BIS) values. After surgery, one group received saline (Group P), while the other received aminophylline (Group A). Results showed that Group A had a faster recovery, with shorter times for eye opening, verbal response, extubation, and arithmetic calculations. Additionally, BIS scores were higher in Group A during the early post-anesthesia period. Although heart rate increased temporarily in Group A, there were no significant differences in blood pressure, oxygen saturation, or anesthesia duration between the two groups.
You can read the abstract of the article at https://onlinelibrary.wiley.com/doi/10.1111/j.0001-5172.2004.00350.x.
Furukawa CT, Duhamel TR, Weimer L, Shapiro GG, Pierson WE, Bierman CW. Cognitive and behavioral findings in children taking theophylline. J Allergy Clin Immunol. 1988;81(1):83-8.
Cognitive and behavioral findings in children taking theophylline
In a follow-up study involving 29 children aged 7 to 12 years (24 boys and five girls), we utilized a double-blind, double-dummy randomized design to investigate the effects of switching from theophylline to cromolyn sodium therapy. Half of the subjects continued to receive theophylline, while the other half was switched to cromolyn sodium therapy. Memory and concentration were assessed using various tests, including the Wechsler Intelligence Scale for Children, Selective Reminding test, Benton Visual Retention test, Stroop tests I and II, and the Child Behavior Checklist. The group receiving cromolyn sodium therapy in place of theophylline demonstrated significant improvements in memory and concentration, particularly in the Stroop test (p < 0.03 by analysis of covariance). Furthermore, there were noteworthy correlations between the duration of theophylline use and scores related to depression (p < 0.03) and obsessive-compulsive behavior (p < 0.04) on the Child Behavior Checklist. These findings reaffirm our earlier pilot study results and raise concerns about the potential long-term side effects of theophylline therapy, including depression and anxiety.
You can read the full article at https://www.jacionline.org/article/0091-6749(88)90224-2/pdf.
Mitrouska I, Kondili E, Prinianakis G, Siafakas N, Georgopoulos D. Effects of theophylline on ventilatory poststimulus potentiation in patients with brain damage. Am J Respir Crit Care Med. 2003;167(8):1124-30.
Effects of theophylline on ventilatory poststimulus potentiation in patients with brain damage
In contrast to normal individuals, patients with brain damage often exhibit a significant decrease in ventilation when brief hypocapnic hypoxia is suddenly replaced with hyperoxia, a phenomenon linked to impaired short-term potentiation activation – a mechanism in the brainstem that promotes breathing stability. Our hypothesis was that theophylline, a drug known to stabilize breathing, might influence short-term potentiation. We conducted a study involving eight stable brain-damaged patients and ten normal adults. The activation of short-term potentiation was assessed by exposing participants to hypoxia followed by hyperoxia after administering either a placebo or theophylline. In both patients and normal subjects, ventilation increased similarly at the
end of hypoxia, regardless of the theophylline treatment. However, in normal subjects, ventilation remained stable when hypoxia abruptly transitioned to hyperoxia, indicating the activation of short-term potentiation. In patients given a placebo, there was a significant undershoot in ventilation during the switch to hyperoxia. Theophylline notably reduced this undershoot, although a slight hypoventilation was still observed compared to normal subjects. These results suggest that theophylline, in patients with brain damage, can largely prevent the drop in ventilation during the transition to hyperoxia, likely by affecting the activation of short-term potentiation, thus explaining its beneficial impact on breathing stability.
You can read the full article at https://www.atsjournals.org/doi/10.1164/rccm.200206-552OC?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Alkana, R. L., Parker, E. S., Cohen, H. B., Birch, H., & Noble, E. P. (1977). Reversal of ethanol intoxication in humans: an assessment of the efficacy of L-dopa, aminophylline, and ephedrine. Psychopharmacology, 55(3), 203–212. https://doi.org/10.1007/BF00497849.
Reversal of ethanol intoxication in humans: an assessment of the efficacy of L-dopa, aminophylline, and ephedrine
We investigated the effects of postethanol treatment with L-Dopa, aminophylline, and/or ephedrine. In one experiment, moderate male drinkers consumed ethanol (0.8 g/kg) followed by either L-Dopa (1.5 g) or a placebo. In a second experiment, subjects consumed ethanol followed by aminophylline (200 mg), ephedrine (50 mg), a combination of aminophylline (200 mg) and ephedrine (50 mg), or a placebo. Both experiments employed double-blind, within-subjects, crossover designs. L-Dopa treatment significantly mitigated ethanol’s effects on the electroencephalogram, motor coordination, and divided attention performance (paired t-test). Similarly, treatment with aminophylline and/or ephedrine significantly reduced ethanol’s impact on the electroencephalogram and motor coordination. These ethanol-antagonizing effects may stem from central noradrenergic stimulation.
You can read the abstract of the article at https://link.springer.com/article/10.1007/BF00497849.
Available from https://jptrm.chitkara.edu.in/index.php/jptrm/article/view/13.
Ghaffaripour S, Khosravi MB, Rahimi A, Sahmedini MA, Chohedri A, Mahmoudi H, Kazemi MR. The effects of Aminophylline on clinical recovery and bispectral index in patients anesthetized with total intravenous anaesthesia. Pak J Med Sci. 2014 Nov-Dec;30(6):1351-5. doi: 10.12669/pjms.306.5853. PMID: 25674137; PMCID: PMC4320729.
The effects of Aminophylline on clinical recovery and bispectral index in patients anesthetized with total intravenous anaesthesia
The objective of this study was to investigate the impact of aminophylline administration on bispectral index (BIS) and clinical recovery in patients undergoing total intravenous anesthesia (TIVA) for inguinal herniorrhaphy. Aminophylline, known for its bronchodilator properties and adenosine antagonism, was administered to one group, while the other received normal saline after anesthesia induction. The results revealed higher heart rate, systolic blood pressure, and BIS scores in the aminophylline group, along with shorter times to eye opening, hand grip, and extubation compared to the control group, demonstrating the potential of aminophylline to expedite recovery in TIVA patients.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4320729/.
Kumral, A., Yesilirmak, D. C., Aykan, S., Genc, S., Tugyan, K., Cilaker, S., Akhisaroglu, M., Aksu, I., Sutcuoglu, S., Yilmaz, O., Duman, N., & Ozkan, H. (2010). Protective effects of methylxanthines on hypoxia-induced apoptotic neurodegeneration and long-term cognitive functions in the developing rat brain. Neonatology, 98(2), 128–136. https://doi.org/10.1159/000278840.
Protective effects of methylxanthines on hypoxia-induced apoptotic neurodegeneration and long-term cognitive functions in the developing rat brain
Aminophylline is commonly used to manage premature apnea, acting as a nonspecific inhibitor of adenosine receptors. However, the effects of methylxanthines like aminophylline on acute brain injury and long-term cognitive functions remain unproven. This study aimed to explore these effects, utilizing newborn rats exposed to intermittent hypoxia and administering intraperitoneal aminophylline during the early postnatal days. The results revealed that aminophylline significantly reduced apoptotic cell numbers in various brain regions and improved long-term neurobehavioral functions, highlighting its potential benefit in mitigating neonatal hypoxic insult in developing rat brains.
You can read the abstract of the article at https://karger.com/neo/article-abstract/98/2/128/228531/Protective-Effects-of-Methylxanthines-on-Hypoxia?redirectedFrom=fulltext.
Available from https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=521007.
Available from https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=323455.
Available from https://journals.lww.com/ejanaesthesiology/Citation/2001/00001/Aminophylline_speeds_recovery_of_halothane.21.aspx.
Kim, D. W., Joo, J. D., In, J. H., Jeon, Y. S., Jung, H. S., Jeon, K. B., Park, J. S., & Choi, J. W. (2013). Comparison of the recovery and respiratory effects of aminophylline and doxapram following total intravenous anesthesia with propofol and remifentanil. Journal of clinical anesthesia, 25(3), 173–176. https://doi.org/10.1016/j.jclinane.2012.07.005.
Comparison of the recovery and respiratory effects of aminophylline and doxapram following total intravenous anesthesia with propofol and remifentanil
In a prospective, randomized, and blinded clinical trial, the effects of aminophylline and doxapram on recovery, respiration, and bispectral index (BIS) values were compared in patients after total intravenous anesthesia (TIVA) with propofol and remifentanil during elective laparoscopic vaginal hysterectomy. Both aminophylline and doxapram shortened the time to spontaneous ventilation and improved early recovery without significant side effects. These drugs also correlated with higher BIS values during emergence, and their arousal and respiratory effects were comparable, suggesting their potential usefulness in facilitating TIVA recovery.
You can read the abstract of the article at https://www.sciencedirect.com/science/article/abs/pii/S095281801300055X?via%3Dihub.
Fischer R, Lang SM, Leitl M, Thiere M, Steiner U, Huber RM. Theophylline and acetazolamide reduce sleep-disordered breathing at high altitude. Eur Respir J. 2004;23(1):47-52.
Theophylline and acetazolamide reduce sleep-disordered breathing at high altitude
In a randomized, double-blind, placebo-controlled study conducted at a high-altitude research laboratory, the effects of theophylline and acetazolamide in treating sleep-disordered breathing (SDB) after rapid ascent to high altitude (3,454 m) were investigated. The study involved 30 healthy male volunteers. Participants received oral slow-release theophylline, oral acetazolamide, or a placebo tablet. Polysomnographic measurements over two consecutive nights revealed highly pathological apnoea/hypopnoea index (AHI) without active medication. Both theophylline and acetazolamide effectively normalized SDB and reduced oxyhaemoglobin desaturations during sleep. Acetazolamide also improved basal oxyhaemoglobin saturation during sleep compared to theophylline. Overall, the study concluded that both medications were effective in addressing high-altitude sleep-disordered breathing.
You can read the full article at https://erj.ersjournals.com/content/23/1/47.long.
Espinoza H, Antic R, Thornton AT, Mcevoy RD. The effects of aminophylline on sleep and sleep-disordered breathing in patients with obstructive sleep apnea syndrome. Am Rev Respir Dis. 1987;136(1):80-4.
In a study involving 10 male patients with obstructive sleep apnea (OSA), the effects of aminophylline and a saline placebo were investigated in a randomized crossover design. The results showed that aminophylline infusion significantly reduced the frequency of apneas containing periods of complete respiratory inactivity (central and mixed apneas) compared to the placebo. However, it had no impact on the frequency or duration of obstructive apneas. While aminophylline showed promise in reducing central apneas, it also disrupted sleep architecture, leading to decreased sleep efficiency, increased sleep fragmentation, and alterations in sleep stages. Therefore, the study concluded that while aminophylline may address central apnea components, it is unlikely to be therapeutically beneficial for OSA patients and may even disrupt sleep patterns, potentially exacerbating upper airway occlusion during sleep.
You can read the abstract of the article at https://www.atsjournals.org/doi/10.1164/ajrccm/136.1.80?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Küpper TE, Strohl KP, Hoefer M, Gieseler U, Netzer CM, Netzer NC. Low-dose theophylline reduces symptoms of acute mountain sickness. J Travel Med. 2008;15(5):307-14.
Low-dose theophylline reduces symptoms of acute mountain sickness
In a double-blind, randomized trial, the efficacy of low-dose, slow-release theophylline in preventing acute mountain sickness (AMS) was investigated. Twenty healthy male volunteers underwent the study, receiving either 300 mg of theophylline daily or a placebo five days prior to ascending to 4,559 m altitude. The results showed that theophylline significantly reduced AMS symptoms compared to the placebo group, as indicated by the Lake Louise Score. Additionally, theophylline was associated with a decrease in periodic breathing events and oxygen desaturations, suggesting its potential to alleviate AMS symptoms and related physiological changes at high altitudes without adverse effects on sleep.
You can read the full article at https://academic.oup.com/jtm/article/15/5/307/1818789?login=false.
Raetzo, M. A., Junod, A. F., & Kryger, M. H. (1987). Effect of aminophylline and relief from hypoxia on central sleep apnoea due to medullary damage. Bulletin europeen de physiopathologie respiratoire, 23(2), 171–175.
Effect of aminophylline and relief from hypoxia on central sleep apnoea due to medullary damage
A 17-year-old boy presented with severe central sleep apneas caused by medullary structural damage. When his oxygen levels dropped, the electroencephalogram displayed sudden slow wave onset. His response to high carbon dioxide levels was weak, and he lacked a response to low oxygen levels. Low-flow oxygen therapy significantly improved his apnea score and duration, potentially by alleviating hypoxic brain depression. Slow waves disappeared with oxygen therapy. Aminophylline proved effective in reducing the apnea score and duration (p < 0.001). These positive effects might be attributed to improvements in normal respiratory oscillations at sleep onset, changes in arousability, or stimulation of the ascending reticular system. These findings suggest that hypoxic depression plays a role in central sleep apneas, and low-flow oxygen and aminophylline can be beneficial treatments for specific cases.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/3607331/.
Louie, G. L., Prokocimer, P. G., Nicholls, E. A., & Maze, M. (1986). Aminophylline shortens thiopental sleep-time and enhances noradrenergic neurotransmission in rats. Brain research, 383(1-2), 377–381. https://doi.org/10.1016/0006-8993(86)90044-2.
Aminophylline shortens thiopental sleep-time and enhances noradrenergic neurotransmission in rats
In our study, we explored how aminophylline impacts thiopental sleep duration and turnover rates of monoamine neurotransmitters in specific brain regions. Rats treated with aminophylline experienced shorter thiopental-induced sleep periods compared to those receiving saline. We observed increased noradrenergic neurotransmission in all brain areas of aminophylline-treated rats under thiopental anesthesia, while turnover rates in other monoaminergic pathways remained unchanged. These findings suggest that acute aminophylline administration enhances central noradrenergic neurotransmission, thereby reducing the hypnotic effect of thiopental.
You can read the abstract of the article at https://www.sciencedirect.com/science/article/abs/pii/0006899386900442?via%3Dihub.
Reiterer, F., Schenkeli, R., Kurz, R., & Haidmayer, R. (1988). Effekt einer Aminophyllintherapie beim reifgeborenen Säugling mit Schlafapnoesyndrom [Effect of aminophylline therapy in mature infants with sleep apnea syndrome]. Monatsschrift Kinderheilkunde : Organ der Deutschen Gesellschaft fur Kinderheilkunde, 136(7), 368–371.
[Effect of aminophylline therapy in mature infants with sleep apnea syndrome]
We conducted a study comparing pneumograms of 33 full-term infants with idiopathic sleep apnea syndrome (SAS), aged 1-16 weeks, who received oral aminophylline treatment, to those of 12 age-matched infants without aminophylline therapy. All infants exhibited pneumogram abnormalities during one-hour oxycardiorespirography, characterized by apneas ≥15 s, ≥3 apneas lasting 10 s, MA-value (mean duration of all apneas during sleep time) ≥7 s/min, and ≥3 episodes of periodic breathing. An SAS diagnosis, considered a potential Sudden Infant Death Syndrome (SIDS) risk factor, was generally made in the presence of clinical symptoms along with abnormal pneumograms. After one week of aminophylline treatment, 88% of infants showed normalized pneumograms, with a mean plasma aminophylline concentration of 8.3 micrograms/ml (range 4-19 micrograms/ml). All abnormalities significantly decreased. In infants without aminophylline, pneumograms remained abnormal, and no significant improvements were observed. After discontinuing aminophylline for at least 6 weeks, followed by one week of monitoring, 83% of infants displayed normal pneumograms, with statistically significant differences compared to initial recordings.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/3211167/.
- Kuzemko JA, Paala J. Apnoeic attacks in the newborn treated with aminophylline. Arch Dis Child. 1973 May;48(5):404-6. doi: 10.1136/adc.48.5.404. PMID: 4703073; PMCID: PMC1648384.
Rudusky BM. Aminophylline: exploring cardiovascular benefits versus medical malcontent. Angiology. 2005;56(3):295-304.
Aminophylline: exploring cardiovascular benefits versus medical malcontent
While aminophylline/theophylline is no longer a primary choice in cardiopulmonary treatment, it can provide substantial benefits in certain pathophysiological conditions, especially those related to cardiac issues. Clinicians should remain cognizant of its potential as an adjunctive therapy, particularly in cases of atrioventricular block, cardiac arrest, heart failure, and bradyarrhythmias. It should not be dismissed as an outdated agent.
You can read the abstract of the article at https://journals.sagepub.com/doi/10.1177/000331970505600309?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Matthay RA. Favorable cardiovascular effects of theophylline in COPD. Chest. 1987;92(1 Suppl):22S-26S.
Favorable cardiovascular effects of theophylline in COPD
Although Theophylline is commonly used as a bronchodilator, recent research indicates its potential to improve cardiovascular performance in individuals with chronic obstructive pulmonary disease (COPD). Whether administered orally as a sustained-release formulation or intravenously as aminophylline, Theophylline has shown the ability to enhance both right and left heart systolic function while reducing pulmonary artery pressure and pulmonary vascular resistance. These positive cardiovascular effects suggest a broader application for Theophylline in COPD treatment, extending beyond its role as a bronchodilator.
You can read the abstract of the article at https://journal.chestnet.org/article/S0012-3692(16)32627-7/fulltext.
Matthay RA. Effects of theophylline on cardiovascular performance in chronic obstructive pulmonary disease. Chest. 1985;88(2 Suppl):112S-117S.
Effects of theophylline on cardiovascular performance in chronic obstructive pulmonary disease
Theophylline, a commonly used bronchodilator, has recently gained recognition for its beneficial cardiovascular effects in patients with chronic obstructive pulmonary disease (COPD). Intravenous aminophylline rapidly lowers pulmonary artery pressures and pulmonary vascular resistance, while increasing both right and left ventricular ejection fraction. Oral long-acting theophylline produces a comparable and lasting enhancement in the performance of both heart ventricles. These improvements are attributed to reduced ventricular afterload and the positive impact of the drug on ventricular contractility. Theophylline may be particularly valuable for individuals dealing with COPD, pulmonary artery hypertension, and concurrent right or left heart failure.
You can read the abstract of the article at https://journal.chestnet.org/article/S0012-3692(16)39217-0/fulltext.
Vestal RE, Eiriksson CE, Musser B, Ozaki LK, Halter JB. Effect of intravenous aminophylline on plasma levels of catecholamines and related cardiovascular and metabolic responses in man. Circulation. 1983;67(1):162-71.
Effect of intravenous aminophylline on plasma levels of catecholamines and related cardiovascular and metabolic responses in man
Theophylline’s mechanism of action, typically attributed to the inhibition of phosphodiesterase leading to increased intracellular cyclic AMP, has been primarily based on in vitro studies using theophylline concentrations much higher than those seen in therapeutic plasma levels. To investigate how theophylline affects the cardiovascular and metabolic systems in relation to sympathetic nervous system activation, intravenous aminophylline was administered to six healthy males under basal conditions. This resulted in a dose-related increase in plasma epinephrine and norepinephrine, heart rate, systolic blood pressure, plasma glucose, free fatty acids, and insulin. While some cardiac parameters were affected by aminophylline, particularly at higher doses, the echocardiographic ejection fraction remained unchanged. These findings suggest that the acute cardiovascular and metabolic effects of theophylline may involve, at least in part, stimulation of the sympathetic nervous system.
You can read the abstract of the article at https://www.ahajournals.org/doi/10.1161/01.cir.67.1.162?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Walther FJ, Sims ME, Siassi B, Wu PY. Cardiac output changes secondary to theophylline therapy in preterm infants. J Pediatr. 1986;109(5):874-6.
Cardiac output changes secondary to theophylline therapy in preterm infants
In this investigation involving 11 clinically stable preterm infants, the cardiovascular impacts of theophylline were assessed. Aminophylline was administered with an initial loading dose of 6.8 mg/kg, followed by a maintenance dose of 2 mg/kg every 8 hours via intravenous infusion. Measurements using pulsed Doppler ultrasound and M-mode echocardiography indicated a significant increase in cardiac output (P < 0.01) and stroke volume (P < 0.02) on days 1, 2, and 3 compared to baseline. By day 7, stroke volume returned to pre-treatment levels, while cardiac output remained elevated. Heart rate showed a consistent and significant increase (P < 0.01) throughout the treatment period, while mean arterial blood pressure remained unchanged. Most of the neonates maintained serum theophylline concentrations between 6 and 13 mg/L. The findings suggest that theophylline therapy in preterm infants has both positive inotropic (increased contractility) and chronotropic (increased heart rate) effects during the initial days of treatment, emphasizing the need for further exploration of the metabolic implications associated with heightened cardiac output.
You can read the abstract of the article at https://www.jpeds.com/article/S0022-3476(86)80717-X/pdf.
Matthay RA, Mahler DA. Theophylline improves global cardiac function and reduces dyspnea in chronic obstructive lung disease. J Allergy Clin Immunol. 1986;78(4 Pt 2):793-9.
Theophylline improves global cardiac function and reduces dyspnea in chronic obstructive lung disease
Theophylline, traditionally recognized as a bronchodilator, has gained attention for its positive cardiovascular effects in chronic obstructive pulmonary disease (CO PD) patients. Intravenous aminophylline administration leads to decreased pulmonary artery pressures, reduced pulmonary vascular resistance, and improved ejection fractions in both right and left ventricles. Similar cardiovascular benefits are observed with oral long-acting theophylline. These improvements in biventricular function may stem from enhanced ventricular contractility and reduced afterload. Recent research has demonstrated that oral theophylline also alleviates dyspnea in COPD patients. Consequently, theophylline could prove beneficial in managing pulmonary artery pressure, treating heart failure, relieving dyspnea, and partially reversing airway obstruction in individuals with COPD.
You can read the full article at https://www.jacionline.org/article/0091-6749(86)90063-1/pdf.
Dutt AK, De soyza ND, Au WY, Hargis JL, Tuck RL. The effect of aminophylline on cardiac rhythm in advanced chronic obstructive pulmonary disease: correlation with serum theophylline levels. Eur J Respir Dis. 1983;64(4):264-70.
The impact of intravenous aminophylline on the cardiac rhythm in advanced, stable chronic obstructive pulmonary disease (COPD) patients was assessed using Holter monitoring in a group of 38 males with an average age of 62 years. Serum levels of aminophylline ranged from 7.4 to 18.6 mg/l. Significant improvements in pulmonary function and blood gases were noted compared to baseline measurements. Only three out of 38 patients (8%) developed new supraventricular tachycardia. Among patients with insignificant ventricular ectopy (VE) at baseline, 76% remained unchanged during therapy. Among those with significant baseline VE, 53% experienced an increase, while 47% had a decrease in VE. No symptomatic arrhythmias were observed. In summary, therapeutic doses of aminophylline did not induce ventricular ectopy in arrhythmia-free COPD patients, but the drug had variable effects on pre-existing VE.
You can read the full article at https://pubmed.ncbi.nlm.nih.gov/6861921/.
Rutherford JD, Vatner SF, Braunwald E. Effects and mechanism of action of aminophylline on cardiac function and regional blood flow distribution in conscious dogs. Circulation. 1981;63(2):378-87.
Effects and mechanism of action of aminophylline on cardiac function and regional blood flow distribution in conscious dogs
The effects of intravenous aminophylline, administered at a rate of 1 mg/kg/min over 10 minutes, were investigated in conscious dogs, focusing on left ventricular (LV) parameters, myocardial contractility indices, and hemodynamics. Aminophylline led to a 12 +/- 2% increase in mean arterial pressure, an 8 +/- 1% rise in LV systolic pressure, a 20 +/- 2% increase in LV dP/dt, a 13 +/- 2% boost in the velocity of myocardial fiber shortening, and a 5 +/- 2% increase in heart rate. Additionally, it reduced LV end-diastolic diameter by 2 +/- 0.5%. Vascular resistance increased in systemic, coronary, mesenteric, and iliac beds by varying degrees but remained unchanged in the renal bed. The positive inotropic effect of aminophylline was partly dependent on intact beta-adrenergic nervous activity and endogenous catecholamine stores, as beta-adrenergic receptor blockade attenuated but did not eliminate this response. Conversely, alpha-adrenergic receptor blockade with phentolamine prevented the aminophylline-induced vasoconstriction in systemic, coronary, mesenteric, and iliac beds. Interestingly, when aminophylline was infused directly into the iliac artery, it induced significant iliac vasodilation, indicating a direct vascular effect. Therefore, intravenous aminophylline, at a dose with minimal impact on heart rate, increased LV contractility and reduced preload in conscious dogs. These actions were influenced by autonomic mechanisms, with beta-adrenergic involvement in the inotropic response and alpha-adrenergic mechanisms mediating the increase in vascular resistance.
You can read the abstract of the article at https://www.ahajournals.org/doi/10.1161/01.cir.63.2.378?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Mokra D, Tonhajzerova I, Mokry J, Petraskova M, Hutko M, Calkovska A. Cardiovascular side effects of aminophylline in meconium-induced acute lung injury. Adv Exp Med Biol. 2013;756:341-7.
Cardiovascular side effects of aminophylline in meconium-induced acute lung injury
To assess the potential side effects of phosphodiesterase inhibitors in the context of neonatal meconium aspiration syndrome (MAS), this study examined blood pressure, heart rate (HR), and heart rate variability (HRV) changes during and after intravenous aminophylline treatment in an animal MAS model. Oxygen-ventilated rabbits received intratracheal meconium (25 mg/ml, 4 ml/kg) or saline, followed by intravenous aminophylline (Syntophyllin, 2 mg/kg) or saline (sham-treated controls) 30 minutes later, with a second dose after 2 hours. In meconium-instilled animals, aminophylline administration led to increased mean arterial blood pressure (MAP), HR, and HRV within 5 minutes, whereas in saline-instilled animals, aminophylline increased HR and showed inconsistent HRV changes compared to sham-treated animals. These cardiovascular parameters gradually returned to baseline within 5 hours after treatment. In conclusion, intravenous aminophylline may induce acute cardiovascular changes, warranting consideration of its potential effects, particularly in MAS patients with cardiovascular instability.
You can read the abstract of the article at https://link.springer.com/chapter/10.1007/978-94-007-4549-0_41.
Roig, E., Magriñá, J., Paz, M., Bassa, P., Recasens, L., Huguet, M., Heras, M., & Sanz, G. (1996). Improvement of exercise-induced ischaemia and myocardial perfusion after aminophylline. Coronary artery disease, 7(1), 69–73.
Improvement of exercise-induced ischaemia and myocardial perfusion after aminophylline
In previous studies, aminophylline has been suggested to improve exercise-induced ischemia by preventing the redistribution of coronary blood flow from ischemic to non-ischemic areas. This study aimed to evaluate whether aminophylline enhances myocardial perfusion in regions supplied by collateral circulation. Twenty-three patients with a blocked coronary artery and collateral circulation from a healthy vessel underwent two symptom-limited exercise tests using 99mTc-MIBI single-photon emission computed tomography (SPECT) myocardial scintigraphy. They received an intravenous infusion of either aminophylline (5 mg/kg over 20 min) or a saline solution in a randomized double-blind procedure. Aminophylline significantly delayed the onset of exercise-induced ischemia in patients with a positive exercise test, increased the rate-pressure product at which ischemia occurred, reduced exercise-induced ST-segment depression, and improved perfusion in collateral-dependent areas. These findings suggest that aminophylline-like drugs could be beneficial for selected patients with ischemic heart disease.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/8773436/.
Hempelmann, G., Frerk, C., Piepenbrock, S., & Schleussner, E. (1978). Beeinflussung von Herzkreislaufparametern durch Aminophyllin (Euphyllin) [Cardio-circulatory effects of aminophylline (Euphyllin) (author’s transl)]. Praktische Anasthesie, Wiederbelebung und Intensivtherapie, 13(5), 437–445.
[Cardio-circulatory effects of aminophylline (Euphyllin) (author’s transl)]
In a study involving 24 patients with congenital or acquired heart disease and functional class II to IV according to the New York Heart Association Classification, the hemodynamic effects of aminophylline were investigated intraoperatively, during extracorporeal circulation, and postoperatively. Aminophylline led to a reduction in arterial pressure, left ventricular pressure, right and left atrial pressure, total systemic resistance, and total pulmonary resistance. Simultaneously, there was an increase in heart peak, peak dp/dt, cardiac index, and stroke index. These findings highlight the favorable cardiac and extracardiac effects of aminophylline in humans.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/362403/.
-
Hemodynamic effects of aminophylline in heart failure
In a study involving nine patients with cardiac failure resulting from hypertensive or coronary heart disease, or a combination of both, right and left heart catheterization was conducted. Hemodynamic assessments were performed both during a control period and following the infusion of 1 gm of aminophylline. Aminophylline consistently and significantly increased cardiac output while significantly decreasing left ventricular end-diastolic pressure, pulmonary artery pressures, and right ventricular end-diastolic pressure. Although the exact mechanism remains uncertain, aminophylline appears to exert a dual effect, stimulating the heart and causing vasodilation, in the context of heart failure.
You can read the abstract of the article at https://www.ajconline.org/article/0002-9149(66)90357-2/fulltext#:~:text=Aminophylline%20produced%20consistent%20and%20significant,right%20ventricular%20end%2Ddiastolic%20pressure..
Goodfellow, J., & Walker, P. R. (1995). Reversal of atropine-resistant atrioventricular block with intravenous aminophylline in the early phase of inferior wall acute myocardial infarction following treatment with streptokinase. European heart journal, 16(6), 862–865. https://doi.org/10.1093/oxfordjournals.eurheartj.a061008.
Reversal of atropine-resistant atrioventricular block with intravenous aminophylline in the early phase of inferior wall acute myocardial infarction following treatment with streptokinase
Three patients experiencing acute inferior myocardial infarction and treated with aspirin (150 mg) and streptokinase (1.5 MU over 60 min) developed atropine-resistant bradyarrhythmias during or immediately after streptokinase administration. Fortunately, these bradyarrhythmias successfully responded to aminophylline, eliminating the necessity for temporary pacing.
You can read the abstract of the article at https://academic.oup.com/eurheartj/article-abstract/16/6/862/457498?redirectedFrom=fulltext&login=false.
Viskin, S., Belhassen, B., Roth, A., Reicher, M., Averbuch, M., Sheps, D., Shalabye, E., & Laniado, S. (1993). Aminophylline for bradyasystolic cardiac arrest refractory to atropine and epinephrine. Annals of internal medicine, 118(4), 279–281. https://doi.org/10.7326/0003-4819-118-4-199302150-00006.
Aminophylline for bradyasystolic cardiac arrest refractory to atropine and epinephrine
In a prospective study, fifteen patients experiencing cardiac arrest, primarily due to asystole or nonperfusing bradyarrhythmias and unresponsive to standard treatments like intravenous atropine and epinephrine, were administered aminophylline (via rapid intravenous injection of 250 mg). A total of 11 out of 15 patients (73%) successfully achieved a stable heart rhythm with sufficient blood pressure for discontinuing closed-chest cardiac massage. All 11 of these patients were alive 60 minutes after resuscitation, with one surviving without neurologic damage. This suggests that aminophylline could potentially improve the immediate outcomes of patients with asystole resistant to standard treatments, prompting further investigation into its potential benefits, particularly when administered earlier during cardiac arrest, for long-term outcomes.
You can read the abstract of the article at https://www.acpjournals.org/doi/10.7326/0003-4819-118-4-199302150-00006?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Melville, K. I., & Lu, F. C. (1950). Effect of epinephrine, aminophylline, nitroglycerine and papaverine on coronary inflow and on heart contraction, as recorded concurrently. The Journal of pharmacology and experimental therapeutics, 99(3), 286–303.
Effect of epinephrine, aminophylline, nitroglycerine and papaverine on coronary inflow and on heart contraction, as recorded concurrently
In experiments with the isolated perfused rabbit heart, continuous recordings were made to observe changes in coronary flow and heart contractions before and after injections of various doses of epinephrine, aminophylline, nitroglycerine, and papaverine. The findings suggest that epinephrine itself does not exert a significant direct effect on coronary vessels but rather affects coronary flow indirectly through myocardial stimulation. Aminophylline, nitroglycerine, and papaverine, on the other hand, induce direct coronary vasodilation when administered in appropriate doses, leading to increased coronary flow per heart beat. Additionally, these drugs have distinct effects on heart rate and contractile amplitudes, which may influence coronary flow rates accordingly.
You can read the abstract of the article at https://jpet.aspetjournals.org/content/99/3/286.long.
Elliott, P. M., Krzyzowska-Dickinson, K., Calvino, R., Hann, C., & Kaski, J. C. (1997). Effect of oral aminophylline in patients with angina and normal coronary arteriograms (cardiac syndrome X). Heart (British Cardiac Society), 77(6), 523–526. https://doi.org/10.1136/hrt.77.6.523
Effect of oral aminophylline in patients with angina and normal coronary arteriograms (cardiac syndrome X)
In this study, 13 patients diagnosed with syndrome X, a condition characterized by exertional angina and normal coronary arteriograms, were examined to assess the efficacy of oral aminophylline. The patients underwent a double-blind crossover trial, receiving either oral aminophylline or a placebo for three weeks each. The results showed that patients who received aminophylline had a longer time to angina during exercise testing compared to the placebo group. However, peak exercise ST depression did not significantly differ between the two groups. Interestingly, some patients on aminophylline reported a reduction in the frequency of chest pain episodes, despite no significant changes in ST segment depression during monitoring. Further investigation is needed to understand these divergent effects on symptoms and ST segment changes in syndrome X patients.
You can read the abstract of the article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC484794/.
Pasnoori, V. R., & Leesar, M. A. (2004). Use of aminophylline in the treatment of severe symptomatic bradycardia resistant to atropine. Cardiology in review, 12(2), 65–68. https://doi.org/10.1097/01.crd.0000096418.72821.fa.
Use of aminophylline in the treatment of severe symptomatic bradycardia resistant to atropine
Bradycardia and cardiac arrest are recognized complications of acute spinal cord injuries, typically of temporary nature. When conventional measures, including correcting hypoxia and administering atropine, prove ineffective, the usual course of action involves considering temporary and permanent pacemaker placement. However, we present two intriguing cases involving severe symptomatic bradycardia resistant to atropine, where the need for pacemaker placement was circumvented through the administration of intravenous aminophylline. Although aminophylline has previously been employed to address resistant bradycardia in various scenarios, such as acute inferior wall myocardial infarction and cardiac transplantation, its use in acute spinal cord injuries is unprecedented. Aminophylline likely exerts its effect in this context by elevating cyclic adenosine monophosphate (cAMP) levels and activating the sympathoadrenal system.
You can read the article at https://journals.lww.com/cardiologyinreview/abstract/2004/03000/use_of_aminophylline_in_the_treatment_of_severe.2.aspx.
Whitman, C. B., Schroeder, W. S., Ploch, P. J., & Raghavendran, K. (2008). Efficacy of aminophylline for treatment of recurrent symptomatic bradycardia after spinal cord injury. Pharmacotherapy, 28(1), 131–135. https://doi.org/10.1592/phco.28.1.131.
Efficacy of aminophylline for treatment of recurrent symptomatic bradycardia after spinal cord injury
Cardiac dysrhythmias and cardiac arrest are potential complications following acute spinal cord injuries (SCI) due to disrupted sympathetic innervation, often resulting in baseline bradycardia. This condition can make individuals vulnerable to vagal stimulation-induced symptomatic bradycardia. While there is limited data on pharmacological interventions for symptomatic bradycardia post-SCI, we present a case of a patient with high cervical SCI experiencing episodic symptomatic bradycardia. The addition of aminophylline to the patient’s treatment regimen successfully resolved the bradycardia. Serum theophylline concentrations in the range of 1.9-3.4 mg/L, consistent with other case reports, were observed during the treatment, highlighting the potential of methylxanthines like aminophylline in preventing episodic bradycardia following SCI. Further research in drug pharmacokinetics and pharmacodynamics in acute SCI patients is warranted to enhance our understanding of this therapeutic approach.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/18154483/.
Murphy, G. W., Schreiner, B. F., Jr, & Yu, P. N. (1968). Effects of aminophylline on the pulmonary circulation and left ventricular performance in patients with valvular heart disease. Circulation, 37(3), 361–369. https://doi.org/10.1161/01.cir.37.3.361.
Effects of aminophylline on the pulmonary circulation and left ventricular performance in patients with valvular heart disease
In a study involving 32 patients with mitral and aortic valvular disease, the effects of intravenous aminophylline on the pulmonary circulation and left ventricular performance were investigated during combined right and transseptal left heart catheterization. Of the 28 patients with complete data, 19 exhibited a decrease in pulmonary vascular distending pressure (PD) along with an increase in pulmonary blood volume (PBV) upon aminophylline infusion, while eight patients showed a drop in PD along with a decline (five patients) or no change (three patients) in PBV. In one case, both PD and PBV increased. This suggests a novel indication of a direct active vasodilating impact of aminophylline on the pulmonary vasculature. Although the cardiac index remained unaffected, the study revealed a positive inotropic effect on the myocardium, marked by a decrease in left ventricular end-diastolic pressure and an increase in the maximum rate of ventricular pressure rise (LV dp/dt). These findings differ from observations in patients with nonvalvular heart failure, where an increase in cardiac index is more commonly noted. The beneficial effects of aminophylline in acute pulmonary edema are attributed to its synergistic impact on the systemic and pulmonary circulations and left ventricular function, collectively contributing to a reduction in PD.
You can read the abstract of the article at https://www.ahajournals.org/doi/10.1161/01.CIR.37.3.361.
Huang D, O’brien RG, Harman E, et al. Does aminophylline benefit adults admitted to the hospital for an acute exacerbation of asthma?. Ann Intern Med. 1993;119(12):1155-60.
Does aminophylline benefit adults admitted to the hospital for an acute exacerbation of asthma
In a randomized, double-blind, placebo-controlled study involving 21 adults hospitalized for acute asthma, the objective was to assess the impact of adding intravenous theophylline (administered as aminophylline) to nebulized albuterol and intravenous methylprednisolone treatment. At admission, the baseline forced expiratory volume in 1 second (FEV1) was 49% ± 19% in the aminophylline group and 43% ± 13% in the placebo group. The aminophylline group showed greater improvement in FEV1 at 3 hours (29% ± 23% compared to 10% ± 10% in the placebo group) and at 48 hours, with FEV1 reaching 75% ± 19% compared to 58% ± 15% in the placebo group. Aminophylline-treated patients required fewer albuterol nebulizations and less total dosage, with no significant differences in asthma symptom scores or adverse effects, indicating that individualized doses of intravenous theophylline, within the therapeutic range, benefit adults hospitalized for acute asthma when added to standard treatment with albuterol and methylprednisolone.
You can read the abstract of the article at https://www.acpjournals.org/doi/10.7326/0003-4819-119-12-199312150-00001?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Mahemuti G, Zhang H, Li J, Tieliwaerdi N, Ren L. Efficacy and side effects of intravenous theophylline in acute asthma: a systematic review and meta-analysis. Drug Des Devel Ther. 2018;12:99-120.
Efficacy and side effects of intravenous theophylline in acute asthma: a systematic review and meta-analysis
In this comprehensive meta-analysis, the use of theophylline, with or without ethylene diamine (aminophylline), for treating acute asthma was assessed. The study analyzed 52 arms from 42 trials and found that theophylline, while reducing heart rate and overall hospital stay compared to certain active controls, was not significantly different in its effects on various parameters like respiratory rate, forced vital capacity, and oxygen saturation. Notably, the efficacy of theophylline was influenced by concomitant medications, with bronchodilators and steroids rendering it a cost-effective and safe choice for acute asthma exacerbations, particularly when considering its affordability and similar efficacy and side effect profile compared to other drugs.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5768195/.
Neame M, Aragon O, Fernandes RM, Sinha I. Salbutamol or aminophylline for acute severe asthma: how to choose which one, when and why?. Arch Dis Child Educ Pract Ed. 2015;100(4):215-22.
Salbutamol or aminophylline for acute severe asthma: how to choose which one, when and why
The management of acute, severe asthma exacerbations poses a significant challenge due to associated morbidity. When initial inhaled and oral treatments prove ineffective, the choice of intravenous therapies becomes critical. This review assesses β-2 agonists and aminophylline, considering their differing mechanisms of action and adverse effect profiles. Evidence from randomized control trials suggests that intravenous salbutamol boluses may alleviate symptoms and expedite recovery. Aminophylline infusions can enhance lung function and, in some cases, symptom relief, but the evidence remains inconclusive. Decisions on treatment selection should factor in risk management, including ease of prescription, preparation, administration, and high-dependency bed availability.
You can read the full article at https://ep.bmj.com/content/100/4/215.long.
Nuhoglu Y, Nuhoglu C. Aminophylline for treating asthma and chronic obstructive pulmonary disease. Expert Rev Respir Med. 2008;2(3):305-13.
Aminophylline for treating asthma and chronic obstructive pulmonary disease
Aminophylline, a theophylline and ethylenediamine combination, primarily relaxes bronchial smooth muscles. Meta-analyses conducted by the Cochrane Collaboration for both children and adults with acute asthma attacks provide differing insights. In children, aminophylline, although not adding significant benefits to standard care, has shown improvements in lung function and reduced intubation risk in a study involving a substantial patient population. Conversely, in adults, aminophylline offers no distinct advantage over standard therapy for acute asthma. In summary, aminophylline may serve as an alternative in children at risk of respiratory fatigue, potentially averting ICU admission and mechanical ventilation. However, due to potential adverse effects, it is not recommended for acute asthma treatment in adults.
You can read the abstract of the article at https://www.tandfonline.com/doi/abs/10.1586/17476348.2.3.305.
Freitag A. Aminophylline injection and theophylline tablets: Acute response in partially reversible chronic airway obstruction. Med J Aust. 1976;1(14):478-9.
Aminophylline injection and theophylline tablets: Acute response in partially reversible chronic airway obstruction
In 10 patients with partially reversible severe airway obstruction, separate administrations of intravenous aminophylline (250 mg) and theophylline tablets (400 mg, Neulin) were compared. Aminophylline was found to be insufficient, with suboptimal plasma theophylline levels and limited ventilatory response. In contrast, oral theophylline achieved an adequate plasma theophylline concentration (10 to 20 µg/ml) within two hours, resulting in consistent improvements in forced expiratory volume in one second (FEV1). Additional significant FEV1 enhancement after salbutamol inhalation indicated that while theophylline tablets consistently improved ventilation, maximal improvement had not been attained.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/933924/.
- Wrenn K, Slovis CM, Murphy F, Greenberg RS. Aminophylline therapy for acute bronchospastic disease in the emergency room. Ann Intern Med. 1991;115(4):241-7.
Aminophylline therapy for acute bronchospastic disease in the emergency room
In a randomized, double-blind, placebo-controlled intervention study, 133 adult patients with asthma or chronic obstructive pulmonary disease experiencing acute exacerbations were evaluated. They all received aerosolized metaproterenol and intravenous methylprednisolone, with 65 patients additionally receiving aminophylline and 68 patients receiving a placebo. Although there were no significant differences in lung function or patient/physician assessments between the two groups, the aminophylline group exhibited a threefold reduction in hospital admission rates (6%) compared to the placebo group (21%). The study suggests that aminophylline, even at slightly subtherapeutic levels, may reduce hospital admissions in acute bronchospastic disease exacerbations, potentially offering substantial cost savings.
You can read the abstract of the article at https://www.acpjournals.org/doi/10.7326/0003-4819-115-4-241?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Rabe KF, Hiemstra PS. Theophylline for chronic obstructive pulmonary disease?.Time to move on. Am J Respir Crit Care Med. 2010;182(7):868-9.
Theophylline for chronic obstructive pulmonary disease?.Time to move on
Chronic obstructive pulmonary disease (COPD) is a significant global health challenge, with a lack of highly effective treatments despite extensive research into its inflammatory mechanisms. While inhaled corticosteroids can provide moderate improvements, they do not cure the inflammation in most patients and have variable effects. In contrast to bronchial asthma, COPD tends to be less responsive to inhaled corticosteroids, a phenomenon known as steroid insensitivity or resistance. Studies have suggested that low-dose theophylline may partially restore steroid sensitivity, possibly through modulation of the PI3K-δ pathway, a crucial signaling pathway linked to inflammation and proliferative diseases. This study presents new evidence regarding the role of PI3K-δ in COPD, indicating that theophylline and selective PI3K-δ inhibitors could help improve steroid responsiveness in COPD, though further clinical evidence is needed to establish their effectiveness. This research marks an important step in understanding the molecular mechanisms involved, potentially paving the way for more targeted interventions in COPD therapy.
You can read the abstract of the article at https://www.atsjournals.org/doi/10.1164/rccm.201008-1271ED?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Shim CS, Williams MH. Bronchodilator response to oral aminophylline and terbutaline versus aerosol albuterol in patients with chronic obstructive pulmonary disease. Am J Med. 1983;75(4):697-701.
Bronchodilator response to oral aminophylline and terbutaline versus aerosol albuterol in patients with chronic obstructive pulmonary disease
In a double-blind crossover study involving 17 patients with stable chronic obstructive pulmonary disease, the bronchodilator effectiveness of oral aminophylline (400 mg) and terbutaline sulfate (5 mg) was compared to the inhalation of three puffs of albuterol sulfate. The results showed that albuterol aerosol provided significantly greater improvements in forced expiratory volume in one second (FEV1) at 30, 60, and 120 minutes compared to oral medications (p < 0.01). Thirteen patients experienced side effects with oral therapy, while none reported side effects with aerosol therapy. Albuterol aerosol achieved maximum bronchodilation in 14 out of 17 patients, with no additional benefit observed from the addition of oral therapy. Consequently, bronchodilator aerosol is recommended as the preferred treatment for chronic obstructive pulmonary disease due to its superior effectiveness and absence of side effects.
You can read the abstract of the article at https://www.amjmed.com/article/0002-9343(83)90459-X/pdf
Ram FS, Jardin JR, Atallah A, et al. Efficacy of theophylline in people with stable chronic obstructive pulmonary disease: a systematic review and meta-analysis. Respir Med. 2005;99(2):135-44.
Efficacy of theophylline in people with stable chronic obstructive pulmonary disease: a systematic review and meta-analysis
In a systematic review of 20 randomized-controlled trials involving people with stable chronic obstructive pulmonary disease (COPD), the efficacy of oral theophylline was compared to placebo. Theophylline demonstrated significant improvements in several outcomes, including FEV1, FVC, VO2 max, PaO2, and PaCO2. Patients expressed a preference for theophylline over placebo, but theophylline increased the risk of nausea. This review underscores that theophylline remains a valuable option in managing stable COPD, but the potential benefits should be considered alongside the associated risks.
You can read the full article at https://www.resmedjournal.com/article/S0954-6111(04)00394-4/fulltext.
Devereux G, Cotton S, Barnes P, et al. Use of low-dose oral theophylline as an adjunct to inhaled corticosteroids in preventing exacerbations of chronic obstructive pulmonary disease: study protocol for a randomised controlled trial. Trials. 2015;16:267. Published 2015 Jun 10. doi:10.1186/s13063-015-0782-2.
Use of low-dose oral theophylline as an adjunct to inhaled corticosteroids in preventing exacerbations of chronic obstructive pulmonary disease: study protocol for a randomised controlled trial
The TWICS trial is a randomized, double-blind, placebo-controlled study taking place in the UK across primary and secondary care sites to investigate the potential clinical and cost-effective benefits of adding “low dose” theophylline to inhaled corticosteroids for individuals with COPD. The trial includes participants with a confirmed diagnosis of COPD, and the primary outcome focuses on the total number of participant-reported COPD exacerbations requiring oral corticosteroids or antibiotics during a 52-week treatment period. This research aims to determine whether this combined treatment approach can reduce exacerbations, offering important insights for patients, clinicians, and healthcare providers in the UK and worldwide.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4465017/.
Devereux G, Cotton S, Fielding S, et al. Effect of Theophylline as Adjunct to Inhaled Corticosteroids on Exacerbations in Patients With COPD: A Randomized Clinical Trial. JAMA. 2018;320(15):1548-1559.
Effect of Theophylline as Adjunct to Inhaled Corticosteroids on Exacerbations in Patients With COPD: A Randomized Clinical Trial
The TWICS trial, a pragmatic, double-blind, placebo-c ontrolled, randomized clinical study, aimed to determine the effectiveness of adding low-dose theophylline to inhaled corticosteroids for patients with COPD. Conducted between February 2014 and August 2016, with the final follow-up ending on August 31, 2017, this study enrolled 1578 participants from 121 UK primary and secondary care sites. The primary outcome measured the number of moderate or severe exacerbations treated with antibiotics, oral corticosteroids, or both over a 1-year treatment period. The results, based on data from 1567 participants, revealed that low-dose theophylline did not significantly reduce the number of COPD exacerbations compared to placebo, concluding that it is not a suitable adjunctive therapy to inhaled corticosteroids for preventing COPD exacerbations.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233797/.
Luo WJ, Ling X, Huang RM. Effects of aminophylline on cytokines and pulmonary function in patients undergoing valve replacement. Eur J Cardiothorac Surg. 2004;25(5):766-71.
Effects of aminophylline on cytokines and pulmonary function in patients undergoing valve replacement
This study aimed to assess the impact of aminophylline on the systemic inflammatory response following cardiopulmonary bypass in patients undergoing valve replacement. Thirty patients were randomly assigned to receive either aminophylline (aminophylline group) or no aminophylline (control group). Aminophylline administration led to significantly lower interleukin-8 and tumor necrosis factor-alpha levels after cardiopulmonary bypass compared to the control group, while interleukin-10 levels were significantly higher. The control group exhibited a greater respiratory index, and the aminophylline group showed lower neutrophil count ratios and plasma malondialdehyde levels. Furthermore, patients in the aminophylline group experienced shorter durations of ventilation and intensive care unit stays. In summary, intraoperative aminophylline administration had an anti-inflammatory effect and improved pulmonary oxygenation in valve replacement patients.
You can read the full article at https://academic.oup.com/ejcts/article/25/5/766/457177?login=false.
Available from https://www.jacionline.org/article/0091-6749(86)90064-3/fulltext.
Chen CY, Yang KY, Lee YC, Perng PP. Effect of oral aminophylline on pulmonary function improvement and tolerability in different age groups of COPD patients. Chest. 2005;128(4):2088-92.
Effect of oral aminophylline on pulmonary function improvement and tolerability in different age groups of COPD patients
This 10-week prospective study aimed to investigate the effects of aminophylline therapy in different age groups of COPD patients. Patients aged 55-74 (group 1) and 75-90 (group 2) received aminophylline treatment. Both groups showed improvements in pulmonary function, with no significant difference between them. Group 1 exhibited a significant increase in peak expiratory flow rate (PEFR), while group 2 did not. Symptom scores improved similarly in both groups, with significantly less chest tightness in group 2. Aminophylline was well-tolerated with no reported electrolyte imbalances or arrhythmias. The study concluded that aminophylline at a standard dose is safe and effective in COPD patients across different age groups, with variations in specific outcomes such as PEFR and chest tightness relief.
You can read the abstract of the article at https://journal.chestnet.org/article/S0012-3692(15)52607-X/fulltext.
Barnes PJ. Theophylline in chronic obstructive pulmonary disease: new horizons. Proceedings of the American Thoracic Society. 2005; 2(4):334-9; discussion 340-1.
Theophylline in chronic obstructive pulmonary disease: new horizons
Emerging evidence suggests that theophylline, typically known for its bronchodilator side effects, exerts significant anti-inflammatory effects in chronic obstructive pulmonary disease (COPD) at lower plasma concentrations. These anti-inflammatory properties are distinct from its actions as a phosphodiesterase inhibitor or adenosine receptor antagonist, which necessitate higher concentrations. Recent research indicates that theophylline, at low therapeutic levels, activates histone deacetylases, enhancing the anti-inflammatory synergy with corticosteroids. Notably, patients with COPD often exhibit reduced histone deacetylase-2, contributing to increased inflammation and steroid resistance. Theophylline has shown promise in restoring steroid sensitivity in vitro, particularly when influenced by oxidative stress. Although the exact mechanism of theophylline’s histone deacetylase activation remains unknown, it operates independently of its known side effects, hinting at the potential for novel drug development.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/16267358/.
Chrystyn H, Mulley BA, Peake MD. Dose response relation to oral theophylline in severe chronic obstructive airways disease. BMJ. 1988;297(6662):1506-10.
Dose response relation to oral theophylline in severe chronic obstructive airways disease
The study aimed to assess the use of trapped gas volume as a measure of respiratory function in patients with chronic obstructive airways disease undergoing theophylline treatment. Patients had their theophylline dosages adjusted based on individual pharmacokinetics for two weeks, followed by random assignment to four consecutive two-month treatment periods (placebo, low, medium, and high theophylline doses). The study found that forced expiratory volume, forced vital capacity, and peak expiratory flow rate showed minimal change across the dosage range. Trapped gas volume, however, exhibited a linear, dose-dependent reduction from placebo to high-dose treatment. The study also observed increased walking distance, a modest improvement in dyspnea, and more frequent minor side effects as the theophylline dose increased. The fall in trapped gas volume suggests an improvement in peripheral ventilation with theophylline treatment, a benefit not as evident in conventional lung function tests for chronic obstructive airways disease patients.
You can read the abstract of the article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1835250/.
Georgopoulos D, Holtby SG, Berezanski D, Anthonisen NR. Aminophylline effects on ventilatory response to hypoxia and hyperoxia in normal adults. J Appl Physiol. 1989;67(3):1150-6.
Aminophylline effects on ventilatory response to hypoxia and hyperoxia in normal adults
In a study involving 10 healthy young adults, ventilation was assessed during hyperoxia with and without aminophylline pretreatment, an adenosine blocker, following two conditions: breathing room air and experiencing 25 minutes of isocapnic hypoxia (reducing arterial oxygen saturation to 80%). Hyperoxia consistently increased inspiratory minute ventilation (VI) in both scenarios. However, during hypoxia, VI initially increased and then decreased below normoxic levels. Aminophylline pretreatment significantly mitigated this hypoxic ventilatory decline. Transitioning to pure oxygen revealed that hyperoxia produced lower VI nadirs at the end of hypoxia compared to room-air breathing, and aminophylline partially prevented this effect. The findings suggest that aminophylline can mitigate the central depression of ventilation during hypoxia but does not influence hyperoxic steady-state hyperventilation, indicating a potential role for adenosine in modulating hypoxic rather than hyperoxic ventilation.
You can read the abstract of the article at https://journals.physiology.org/doi/abs/10.1152/jappl.1989.67.3.1150?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org.
Lim S, Tomita K, Caramori G, et al. Low-dose theophylline reduces eosinophilic inflammation but not exhaled nitric oxide in mild asthma. Am J Respir Crit Care Med. 2001;164(2):273-6.
Low-dose theophylline reduces eosinophilic inflammation but not exhaled nitric oxide in mild asthma
In a double-blind, placebo-controlled crossover study involving 15 patients with mild asthma who were not receiving inhaled steroid therapy, the impact of low-dose theophylline treatment (250 mg twice daily) on inflammatory markers was investigated. The results revealed that low-dose theophylline led to a significant reduction in sputum eosinophils, bronchoalveolar lavage eosinophils, and biopsy eosinophils, from 11.3%, 3.4%, and 1.83% to 8.0%, 1.7%, and 1.20%, respectively. However, there were no significant changes in exhaled nitric oxide levels or improvements in lung function and bronchial responsiveness. This suggests that low-dose theophylline exhibits anti-inflammatory effects in asthma by reducing airway eosinophils without affecting exhaled nitric oxide or lung function.
You can read the full article at https://www.atsjournals.org/doi/10.1164/ajrccm.164.2.2006043?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Sullivan P, Bekir S, Jaffar Z, Page C, Jeffery P, Costello J. Anti-inflammatory effects of low-dose oral theophylline in atopic asthma. Lancet. 1994;343(8904):1006-8.
Anti-inflammatory effects of low-dose oral theophylline in atopic asthma
In a double-blind, placebo-controlled study involving 19 atopic asthmatic subjects, we investigated the impact of oral theophylline on the bronchial mucosa’s inflammatory response to allergen inhalation. Bronchoscopy and bronchial biopsy were conducted 24 hours after allergen exposure both before and after six weeks of treatment with oral slow-release theophylline at 200 mg every 12 hours. Despite maintaining serum concentrations below the commonly-accepted therapeutic range, theophylline treatment resulted in a significant reduction in the number of EG2-positive activated eosinophils (5.9 before and 2.1 after treatment, p < 0.05) and total eosinophils (16.7 before and 7.6 after treatment, p < 0.05) beneath the epithelial basement membrane. In conclusion, low-dose oral theophylline mitigates the airway’s inflammatory response to allergen inhalation in atopic asthma.
You can read the abstract of the article at https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(94)90127-9/fulltext.
Parker, J. O., Kelkar, K., & West, R. O. (1966). Hemodynamic effects of aminophylline in cor pulmonale. Circulation, 33(1), 17–25. https://doi.org/10.1161/01.cir.33.1.17.
Hemodynamic effects of aminophylline in cor pulmonale
Nine patients with cor pulmonale resulting from chronic obstructive pulmonary disease underwent right and left heart catheterization. During the study, observations were made under normal conditions and while receiving a 1 g infusion of aminophylline. Aminophylline led to a significant reduction in mean pulmonary artery pressure, right ventricular end-diastolic pressure, left ventricular end-diastolic pressure, and brachial artery mean pressure. While heart rate and oxygen consumption increased, there was no change in cardiac index. Furthermore, alveolar ventilation significantly increased. These findings suggest that the decrease in pulmonary artery pressure was likely due to pulmonary arteriolar dilation.
You can read the full article at
Fairfax, A. J., McNabb, W. R., Davies, H. J., & Spiro, S. G. (1980). Slow-release oral salbutamol and aminophylline in nocturnal asthma: relation of overnight changes in lung function and plasma drug levels. Thorax, 35(7), 526–530. https://doi.org/10.1136/thx.35.7.526.
Slow-release oral salbutamol and aminophylline in nocturnal asthma: relation of overnight changes in lung function and plasma drug levels
In a double-blind controlled trial involving 14 chronic asthmatic patients experiencing regular nocturnal exacerbations, 16 mg of slow-release oral salbutamol (equivalent to two Ventolin spandets), 450 mg of slow-release aminophylline (equivalent to two Phyllocontin Continus tablets), or a placebo was administered at midnight. The mean peak expiratory flow rates upon awakening were significantly higher with the active drugs compared to placebo (p < 0.01 for salbutamol; p < 0.05 for aminophylline), although neither drug completely eliminated the overnight decrease in PEFR. Plasma drug levels at 0600 hr were 17.3 ng/ml (+/- 5.3 ng/ml SD) for salbutamol and 7.1 micrograms/ml (+/- 3.1 micrograms/ml SD) for theophylline. Calculations based on steady-state plasma levels suggested that the morning salbutamol levels were likely within the therapeutic range for asthma. However, the morning theophylline levels were suboptimal when aminophylline was administered only at night.
You can read the abstract of the article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC471327/.
Barrett, C. T., Sevanian, A., Phelps, D. L., Gilden, C., & Kaplan, S. A. (1978). Effects of cortisol and aminophylline upon survival, pulmonary mechanics, and secreted phosphatidyl choline of prematurely delivered rabbits. Pediatric research, 12(1), 38–42. https://doi.org/10.1203/00006450-197801000-00010.
Effects of cortisol and aminophylline upon survival, pulmonary mechanics, and secreted phosphatidyl choline of prematurely delivered rabbits
Rabbits delivered at 27.0 days of gestation were subjected to a study involving cortisol (2 mg/kg/day), aminophylline (6.25 mg/kg/day), or sterile saline administration to does on days 24-26 of gestation. When assessed for survival at 60 minutes in a warm, oxygen-enriched environment with frequent tactile stimulation, the aminophylline-treated group exhibited a survival rate of 52.9%, while the control and cortisol-treated groups had a rate of 22.2%. In animals surviving for 60 minutes, the cortisol-treated group showed lower lung volume at 30 cm H2O compared to the controls or the aminophylline-treated group. Furthermore, the aminophylline-treated group retained more gas at lower pressures on the deflation curve and had a greater amount of phosphatidylcholine recovered in lung lavage fluid than the other groups. In this experimental model, aminophylline appeared to enhance lung maturation more effectively than cortisol.
You can read the abstract of the article at https://www.nature.com/articles/pr197810.
Sevanian, A., Gilden, C., Kaplan, S. A., & Barrett, C. T. (1979). Enhancement of fetal lung surfactant production by aminophylline. Pediatric research, 13(12), 1336–1340. https://doi.org/10.1203/00006450-197912000-00007.
Enhancement of fetal lung surfactant production by aminophylline
Antepartum administration of aminophylline to pregnant rabbits led to an accelerated formation of phospholipids, which are considered crucial components of pulmonary surfactant. Lung slice preparations from treated fetuses showed increased tissue content and synthesis of saturated phosphatidylcholine and phosphatidylinositol, as measured using labeled palmitate, oleate, and glucose as precursors. The results indicated heightened de novo production of these lipids, with glucose and glycogen potentially serving as significant precursors. While there was a notable reduction in triglyceride content and an increase in free fatty acids, suggesting increased lipolysis in the aminophylline-treated groups, this did not substantially impact the rate of labeled palmitate incorporation into total phospholipids.
You can read the full article at https://www.nature.com/articles/pr1979474.
Chapman, D. L., Carlton, D. P., Cummings, J. J., Poulain, F. R., & Bland, R. D. (1991). Intrapulmonary terbutaline and aminophylline decrease lung liquid in fetal lambs. Pediatric research, 29(4 Pt 1), 357–361. https://doi.org/10.1203/00006450-199104000-00006.
Intrapulmonary terbutaline and aminophylline decrease lung liquid in fetal lambs
To investigate the potential enhancement of beta-adrenergic stimulation on fetal lung liquid secretion through phosphodiesterase inhibition, fetal lambs with chronically placed tracheal loop catheters were studied. The independent and combined effects of intrapulmonary terbutaline and aminophylline on net production of lung luminal liquid over time (Jv) were examined. Terbutaline (10(-5) M) reduced Jv from 11 +/- 1 to -3 +/- 2 mL/h in 21 experiments, while aminophylline (10(-3) M) alone had no significant effect in six other studies. When the two drugs were administered sequentially, terbutaline initially decreased Jv, and aminophylline further decreased Jv. Amiloride (10(-4) M), an inhibitor of epithelial Na+ transport, reversed the combined effect of terbutaline and aminophylline, increasing Jv. This suggests that phosphodiesterase inhibition amplifies the beta-adrenergic impact of terbutaline on Na(+)-dependent absorption of lung luminal liquid in fetal lambs.
You can read the full article at https://www.nature.com/articles/pr199170.
Gross, I., & Rooney, S. A. (1977). Aminophylline stimulates the incorporation of choline into phospholipid in explants of fetal rat lung in organ culture. Biochimica et biophysica acta, 488(2), 263–269. https://doi.org/10.1016/0005-2760(77)90183-7.
Aminophylline stimulates the incorporation of choline into phospholipid in explants of fetal rat lung in organ culture
We examined the direct impact of aminophylline, a cyclic AMP phosphodiesterase inhibitor, and cyclic AMP on choline incorporation into phospholipids in organ-cultured explants of fetal rat lung. Explants from 19-day fetal rat lung were cultured for 24 or 48 hours in the presence of aminophylline or dibutyryl cyclic AMP, with control explants cultured in medium alone. Aminophylline exposure led to an 88% increase in choline incorporation into phosphatidylcholine and a 95% increase in sphingomyelin after 48 hours, with similar changes observed after 24 hours. There was a small increase in the percentage of synthesized disaturated phosphatidylcholine. Explants cultured with cyclic AMP showed a 77% and 53% stimulation in choline incorporation into phosphatidylcholine and sphingomyelin, respectively. These findings suggest that aminophylline directly stimulates choline incorporation into phospholipids in fetal rat lung, likely through cyclic AMP mediation.
You can read the abstract of the article at https://www.sciencedirect.com/science/article/abs/pii/0005276077901837?via%3Dihub.
Cosmi, E. V., Saitto, C., Barbati, A., Del Bolgia, F., Di Renzo, G. C., Grossmann, G., Lachmann, B., & Robertson, B. (1986). Effect of aminophylline on lung maturation in preterm rabbit fetuses. American journal of obstetrics and gynecology, 154(2), 436–439. https://doi.org/10.1016/0002-9378(86)90686-1.
Effect of aminophylline on lung maturation in preterm rabbit fetuses
Pregnant rabbit does received intravenous aminophylline (6 mg/kg/day) from the twenty-fifth day after mating, and the fetuses were delivered on the twenty-eighth day. Newborn rabbits were divided into two groups: one breathed air, the other 100% oxygen. Aminophylline-treated newborns exhibited higher body weights, improved survival rates, and increased lung lavage fluid phosphatidylglycerol levels. While aminophylline-treated animals breathing air had higher respiratory frequency, lung compliance did not significantly differ from controls. The beneficial effects of aminophylline in this model were mainly due to accelerated fetal growth and improved postnatal breathing regulation, with less specific influence on lung maturation, both functionally and biochemically.
You can read the abstract of the article at https://www.ajog.org/article/0002-9378(86)90686-1/pdf.
Maniscalco, W. M., Wilson, C. M., & Gross, I. (1979). Influence of aminophylline and cyclic AMP on glycogen metabolism in fetal rat lung in organ culture. Pediatric research, 13(12), 1319–1322. https://doi.org/10.1203/00006450-197912000-00003.
Influence of aminophylline and cyclic AMP on glycogen metabolism in fetal rat lung in organ culture
In 19-day fetal rat lung explants cultured for 24 hours, aminophylline, a cyclic adenosine 3′,5′ monophosphate (AMP) phosphodiesterase inhibitor, and dibutyryl cyclic AMP reduced the glycogen content by 25% (p < 0.025) and 75% (p < 0.001), respectively. Both treatments also decreased the activity of glycogen synthase I by 32% in aminophylline-treated cultures (p < 0.025) and 25% in cyclic AMP-treated cultures (p < 0.025). The proportion of active synthase significantly decreased in all treated cultures, while glycogen phosphorylase a and total phosphorylase activity remained unaffected. These results indicate that aminophylline and cyclic AMP have an impact on glycogen metabolism in fetal rat lung explants during organ culture.
You can read the full article at https://www.nature.com/articles/pr1979470.
Mokra, D., Drgova, A., Mokry, J., Bulikova, J., Pullmann, R., Durdik, P., Petraskova, M., & Calkovska, A. (2008). Combination of budesonide and aminophylline diminished acute lung injury in animal model of meconium aspiration syndrome. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society, 59 Suppl 6, 461–471.
Combination of budesonide and aminophylline diminished acute lung injury in animal model of meconium aspiration syndrome
The combination of low-dose budesonide and low-dose aminophylline shows promise for improving lung function while minimizing adverse effects compared to high-dose monotherapy. In an experiment using adult rabbits exposed to meconium, those treated with aminophylline alone exhibited some respiratory improvements, whereas the combination of budesonide and aminophylline proved more effective in reducing intrapulmonary shunts and enhancing gas exchange, without significant cardiovascular impacts. Combined treatment also led to greater reductions in lung edema and lung neutrophil count compared to aminophylline alone. Both treatments reduced lung peroxidation and airway reactivity to histamine, with aminophylline alone showing a stronger effect. The combination of budesonide and aminophylline enhanced respiratory parameters more effectively while having fewer side effects than aminophylline alone, although no additional benefits were observed in terms of lung peroxidation and airway reactivity.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/19218670/.
Mokra, D., Mokry, J., Tatarkova, Z., Redfors, B., Petraskova, M., & Calkovska, A. (2007). Aminophylline treatment in meconium-induced acute lung injury in a rabbit model. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society, 58 Suppl 5(Pt 1), 399–407.
Aminophylline treatment in meconium-induced acute lung injury in a rabbit model
Administration of methylxanthines may mitigate meconium-induced acute lung injury. In a study involving meconium-instilled rabbits, aminophylline was intravenously administered at two doses 0.5 hours and 2.5 hours after meconium instillation, while control rabbits received no treatment, followed by 5 hours of oxygen ventilation. Aminophylline led to significant improvements in gas exchange, reduced right-to-left pulmonary shunts, lowered central venous pressure, and decreased ventilatory pressures within 5 hours after the first dose. Furthermore, aminophylline reduced meconium-induced lung edema formation, airway hyperreactivity to histamine, neutrophil count in bronchoalveolar lavage fluid, and oxidative modifications of proteins and lipids in lung tissue, compared to the untreated meconium-instilled group. In a rabbit model of meconium aspiration syndrome, aminophylline treatment enhanced pulmonary functions and mitigated oxidative injury and changes in airway reactivity associated with lung inflammation.
You can read the full article at https://www.jpp.krakow.pl/journal/archive/11_07_s5/pdf/399_11_07_s5_article.pdf
Mokra, D., Drgova, A., Mokry, J., Pullmann, R., Redfors, B., Petraskova, M., & Calkovska, A. (2008). Comparison of the effects of low-dose vs. high-dose aminophylline on lung function in experimental meconium aspiration syndrome. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society, 59 Suppl 6, 449–459.
Comparison of the effects of low-dose vs. high-dose aminophylline on lung function in experimental meconium aspiration syndrome
Due to the lack of information on appropriate aminophylline dosing in meconium aspiration syndrome (MAS), this study compared the effects of high-dose (HD) and low-dose (LD) aminophylline on lung function in animals with MAS. Meconium-instilled rabbits received either LD-aminophylline (1.0 mg/kg) or HD-aminophylline (2.0 mg/kg) at 0.5 and 2.5 hours after meconium instillation, or were untreated. Within 5 hours of oxygen ventilation, HD-aminophylline significantly improved gas exchange, reduced pulmonary shunts and ventilatory pressures, and decreased edema formation and lung neutrophils. LD-aminophylline improved lung function to a lesser extent than HD-aminophylline and failed to reduce lung edema and the number of lung neutrophils. Both treatments reduced lung peroxidation, with HD-aminophylline more effectively affecting lipid oxidation and LD-aminophylline having a stronger impact on protein oxidation. Tracheal reactivity to histamine decreased after HD-aminophylline, while lung tissue reactivity was more reduced after LD-aminophylline. Although LD-aminophylline exhibited some anti-inflammatory potential, HD-aminophylline proved more effective in improving most parameters.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/19218669/.
Lindenschmidt, R. C., & Witschi, H. (1985). Attenuation of pulmonary fibrosis in mice by aminophylline. Biochemical pharmacology, 34(24), 4269–4273. https://doi.org/10.1016/0006-2952(85)90283-7.
Attenuation of pulmonary fibrosis in mice by aminophylline
Cyclic nucleotides have been shown in vitro to regulate fibroblast proliferation and collagen production. A previous study demonstrated that propranolol, which decreases the cAMP/cGMP ratio, increases fibrosis in a damaged lung. This study aimed to determine if increasing the cAMP/cGMP ratio could reduce collagen production by fibroblasts after lung damage. Lung injury was induced in mice using butylated hydroxytoluene (BHT) or bleomycin, and a phosphodiesterase inhibitor, aminophylline, was administered. Aminophylline, which elevated the cAMP/cGMP ratio, attenuated the increase in total lung collagen following injury, suggesting that increasing the cAMP/cGMP ratio early in the damage and repair process correlates with reduced hydroxyproline deposition.
You can read the abstract of the article at https://www.sciencedirect.com/science/article/abs/pii/0006295285902837?via%3Dihub.
Wanke, T., Merkle, M., Zifko, U., Formanek, D., Lahrmann, H., Grisold, W., & Zwick, H. (1994). The effect of aminophylline on the force-length characteristics of the diaphragm. American journal of respiratory and critical care medicine, 149(6), 1545–1549. https://doi.org/10.1164/ajrccm.149.6.8004311.
The effect of aminophylline on the force-length characteristics of the diaphragm
Our study aimed to assess the impact of aminophylline on human diaphragm contractile function at different muscle fiber lengths. Ten healthy subjects underwent maximal sniff maneuvers and bilateral phrenic nerve twitch stimulations, with or without intravenous aminophylline infusion in a randomized manner. Aminophylline did not affect the contractility of the fresh diaphragm at various lung volumes. However, in the exhausted diaphragm, aminophylline significantly improved pressure values generated by sniffs and twitch stimulations, even at lung volumes of 60%, 75%, and 90% of total lung capacity. This enhancement of diaphragm contractility occurred irrespective of neuronal firing rates, whether low (twitch stimulation) or high (sniff maneuver).
You can read the abstract of the article at https://www.atsjournals.org/doi/10.1164/ajrccm.149.6.8004311?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Aubier, M., De Troyer, A., Sampson, M., Macklem, P. T., & Roussos, C. (1981). Aminophylline improves diaphragmatic contractility. The New England journal of medicine, 305(5), 249–252. https://doi.org/10.1056/NEJM198107303050503.
Aminophylline improves diaphragmatic contractility
To elucidate the clinical effectiveness of aminophylline, we examined its impact on diaphragmatic function in eight healthy individuals. We assessed the relationship between diaphragm electrical activity and the resulting pressure during voluntary contractions before and after aminophylline infusion. Aminophylline caused a leftward shift in the electrical activity/pressure curve, leading to an average 15% increase in pressure at a given electrical activity (P < 0.001). In four subjects, pressure was measured during phrenic nerve stimulation at different frequencies before and after inducing diaphragmatic fatigue through resistive breathing, both with and without aminophylline infusion. Following fatigue, pressure increased at all stimulation frequencies with aminophylline, compared to pressure after similar fatigue runs without aminophylline, with a mean plasma aminophylline concentration of 13 ± 0.9 mg per liter. In conclusion, aminophylline enhances diaphragm contractility and reduces its susceptibility to fatigue.
You can read the abstract of the article at https://www.nejm.org/doi/10.1056/NEJM198107303050503?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Kennedy, T. P., Michael, J. R., Hoidal, J. R., Hasty, D., Sciuto, A. M., Hopkins, C., Lazar, R., Bysani, G. K., Tolley, E., & Gurtner, G. H. (1989). Dibutyryl cAMP, aminophylline, and beta-adrenergic agonists protect against pulmonary edema caused by phosgene. Journal of applied physiology (Bethesda, Md. : 1985), 67(6), 2542–2552. https://doi.org/10.1152/jappl.1989.67.6.2542.
Dibutyryl cAMP, aminophylline, and beta-adrenergic agonists protect against pulmonary edema caused by phosgene
Phosgene is a hazardous oxidant gas responsible for inducing adult respiratory distress syndrome in exposed workers. It leads to a significant increase in lung weight gain in buffer-perfused isolated rabbit lungs (31 ± 5 g over 60 min after phosgene exposure compared to 7.7 ± 1.2 in control lungs, P < 0.01) and a substantial rise in the lung leak index for 125I-albumin (0.28 ± 0.03 after phosgene vs. 0.02 ± 0.01 in control lungs, P < 0.01). Pretreatment with dibutyryl adenosine 3′,5′ -cyclic monophosphate (DBcAMP), aminophylline, or terbutaline plus isoproterenol effectively prevented the phosgene-induced lung weight increase (31 ± 5 g phosgene, 11.7 ± 2.8 DBcAMP, 7.5 ± 2.5 aminophylline, 6.1 ± 1 terbutaline and isoproterenol, 6.1 ± 1.2 control + aminophylline, and 7.7 ± 1.2 control; all treatments P < 0.01 compared to the untreated phosgene group and not significantly different from control lungs). Aminophylline pretreatment also prevented the surge in the lung leak index for 125I-albumin (0.28 ± 0.03 after phosgene vs. 0.06 ± 0.02 in aminophylline-treated lungs, P < 0.01). Posttreatment with aminophylline and terbutaline likewise prevented the phosgene-induced lung weight increase. These findings demonstrate that phosgene significantly augments fluid and protein movement across the pulmonary vasculature and that treatment with DBcAMP, aminophylline, terbutaline, or isoproterenol substantially mitigates the pulmonary edema resulting from phosgene exposure.
You can read the abstract of the article at https://journals.physiology.org/doi/abs/10.1152/jappl.1989.67.6.2542?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org.
Mizus, I., Summer, W., Farrukh, I., Michael, J. R., & Gurtner, G. H. (1985). Isoproterenol or aminophylline attenuate pulmonary edema after acid lung injury. The American review of respiratory disease, 131(2), 256–259. https://doi.org/10.1164/arrd.1985.131.2.256.
Isoproterenol or aminophylline attenuate pulmonary edema after acid lung injury
We investigated whether isoproterenol and aminophylline could mitigate both the pulmonary hypertension and the increased pulmonary vascular permeability resulting from the intratracheal instillation of hydrochloric acid. Using blood-perfused isolated rabbit lungs, we measured changes in pulmonary artery pressure and lung weight for 30 minutes after acid injury (2 ml/kg 0.1 N HCl). In a control group without acid injury, pulmonary artery pressure and lung weight remained constant throughout 1 hour of perfusion. In an acid control group, pulmonary artery pressure increased by 11 ± 3 mmHg (p < 0.01), and lung weight increased by 19.2 ± 5.1 g over 30 minutes following acid injury (p < 0.001). Pretreatment with aminophylline (p < 0.01) or isoproterenol (p < 0.001) effectively prevented the increase in pulmonary artery pressure after acid instillation. Aminophylline pretreatment significantly reduced the increase in lung weight caused by acid injury to 3.6 ± 1.0 g over 30 minutes (p < 0.01). Isoproterenol pretreatment prevented any increase in lung weight (0.5 ± 0.5 g over 30 minutes, p < 0.01). Post-treatment with isoproterenol, initiated 3 minutes after acid instillation, also prevented the increase in pulmonary artery pressure (p < 0.01) and markedly reduced the increase in lung weight to 5.8 ± 2.4 g over 30 minutes (p < 0.01). Isoproterenol’s beneficial effect is mediated through beta-adrenergic receptor activation, as propranolol reverses its effect.
You can read the abstract of the article at https://www.atsjournals.org/doi/10.1164/arrd.1985.131.2.256?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Sciuto, A. M., Strickland, P. T., Kennedy, T. P., & Gurtner, G. H. (1997). Postexposure treatment with aminophylline protects against phosgene-induced acute lung injury. Experimental lung research, 23(4), 317–332. https://doi.org/10.3109/01902149709039229.
Postexposure treatment with aminophylline protects against phosgene-induced acute lung injury
Pretreatment with aminophylline has been known to protect against various forms of acute lung injury. While the mechanisms involved are complex, they are believed to relate to cAMP upregulation. Unlike previous studies that focused on pretreatment, this research explored post-treatment in rabbits exposed to a lethal dose of the oxidant gas phosgene. Post-treatment with aminophylline, administered 80-90 minutes after exposure, significantly reduced pulmonary artery pressure (Ppa), tracheal pressure (Pt), and lung weight gain (lwg). Aminophylline also lowered thiobarbituric acid-reactive substances (TBARS), perfusate leukotrienes C4/D4/E4 (LTC4/D4/E4), and prevented phosgene-induced reductions in lung tissue cAMP. These findings suggest that aminophylline’s protective mechanisms involve reduced LTC4/D4/E4-mediated pulmonary capillary permeability, decreased lipid peroxidation, and potentially direct anti-permeability effects of cAMP on cellular contraction in guarding against phosgene-induced lung injury.
You can read the full article at https://www.tandfonline.com/doi/abs/10.3109/01902149709039229.
Nowak, D., Rozniecki, J., Ruta, U., Bednarowicz, A., & Izdebski, J. (1988). The influence of aminophylline on human neutrophils–possible protection of lung from proteolytic injury. Archivum immunologiae et therapiae experimentalis, 36(3), 351–360.
The influence of aminophylline on human neutrophils–possible protection of lung from proteolytic injury
The imbalance between proteases and antiproteases in the lungs is a likely contributor to lung injuries such as emphysema. Aminophylline, commonly used in conditions like bronchitis, bronchial asthma, and emphysema, was investigated in vitro to assess its impact at therapeutic concentrations (12 and 20 micrograms/ml) on various neutrophil functions. It was found that aminophylline did not significantly affect phagocytosis, leukoprotease, or acid phosphatase release. However, it led to a decrease in total protein release (p < 0.02 at 12 micrograms/ml and p < 0.02 at 20 micrograms/ml), with an average reduction of 13.5% compared to the control. Aminophylline also inhibited the release of proteins with a molecular weight below 35,000 daltons. Additionally, it caused significant inhibition of neutrophil migration (22% at 12 micrograms/ml and 53% at 20 micrograms/ml) and reduced neutrophil chemotaxis (p < 0.02 at 12 micrograms/ml and p < 0.05 at 20 micrograms/ml). These findings suggest that at higher doses, aminophylline may reduce the inflammatory recruitment of neutrophils, which are a potential source of elastase in the lung, thus potentially diminishing proteolytic lung injury.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/3074741/.
Mitra, A., Bassler, D., Goodman, K., Lasserson, T. J., & Ducharme, F. M. (2005). Intravenous aminophylline for acute severe asthma in children over two years receiving inhaled bronchodilators. The Cochrane database of systematic reviews, 2005(2), CD001276. https://doi.org/10.1002/14651858.CD001276.pub2.
Intravenous aminophylline for acute severe asthma in children over two years receiving inhaled bronchodilators
Given the evolution of treatments like inhaled beta2-agonists, anticholinergic agents, and glucocorticoids, the role of aminophylline in pediatric acute asthma has become less clear. Nevertheless, there is some consensus that it may be beneficial for children with acute severe asthma who are already receiving maximal therapy, including oxygen, inhaled bronchodilators, and glucocorticoids. A review of seven trials involving 380 participants found that the addition of intravenous aminophylline to beta2-agonists and glucocorticoids improved lung function within 6 hours of treatment but did not significantly reduce symptoms, the frequency of nebulizations, or the length of hospital stays. There wasn’t enough data to evaluate its impact on oxygenation, admission to the pediatric intensive care unit (PICU), or the need for mechanical ventilation. However, aminophylline was associated with a three-fold increase in the risk of vomiting, and no significant differences were observed between treatment groups regarding other side effects or mortality.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7027703/.
Protective Effect of Aminophylline against Cigarette Smoke Extract–Induced Apoptosis in Human Lung Fibroblasts (MRC-5 Cells).
Protective Effect of Aminophylline against Cigarette Smoke Extract–Induced Apoptosis in Human Lung Fibroblasts (MRC-5 Cells)
Cigarette smoking, a leading cause of chronic obstructive pulmonary disease (COPD) and emphysema, triggers apoptosis (cell death) in lung structural cells. Xanthine derivatives like aminophylline, used as a bronchodilator in COPD treatment, have unclear effects on lung cell apoptosis. This study explored aminophylline’s impact on cigarette smoke extract (CSE)-induced apoptosis in lung fibroblasts. Aminophylline, particularly at 10 μg/ml concentration, significantly enhanced cell viability after 8-hour exposure to 20% CSE. Pre-treatment with aminophylline (10 μg/ml) decreased Annexin staining from 68% to 12% after 12-hour 20% CSE exposure. Additionally, aminophylline reduced caspase 3 and 8 activities and nuclear condensation/fragmentation, suggesting its potential as an agent to counter cigarette smoke-induced lung cell apoptosis.
You can read the full article at https://onlinelibrary.wiley.com/doi/10.1111/j.1742-7843.2011.00673.x.
Armanian AM, Badiee Z, Afghari R, Salehimehr N, Hassanzade A, Sheikhzadeh S, Shariftehrani M, Rezvan G. Reducing the incidence of chronic lung disease in very premature infants with aminophylline. Int J Prev Med. 2014 May;5(5):569-76. PMID: 24932388; PMCID: PMC4050677.
Reducing the incidence of chronic lung disease in very premature infants with aminophylline
In this long-term randomized clinical trial, the study aimed to evaluate the safety and preventive impact of aminophylline on the development of chronic lung disease (CLD) in extremely premature infants. The study group received aminophylline during the first 10 days of life, while the control group did not. Results showed that premature infants treated with aminophylline had significantly shorter periods of oxygen dependency, with a median duration of 3 days compared to 14 days in the control group. Moreover, the incidence of CLD was significantly lower in the aminophylline group, with only 8.7% of infants developing CLD, compared to 44% in the control group. No adverse effects were reported. This study highlights the preventive benefits of aminophylline, particularly in very premature infants, in reducing the occurrence of CLD.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4050677/.
Hadjigeorgiou, E., Kitsiou, S., Psaroudakis, A., Segos, C., Nicolopoulos, D., & Kaskarelis, D. (1979). Antepartum aminophylline treatment for prevention of the respiratory distress syndrome in premature infants. American journal of obstetrics and gynecology, 135(2), 257–260. https://doi.org/10.1016/0002-9378(79)90355-7.
Antepartum aminophylline treatment for prevention of the respiratory distress syndrome in premature infants
The study assessed the incidence of idiopathic respiratory distress (IRD) in prematurely born infants when their mothers received aminophylline before the thirty-fourth week of pregnancy. In the aminophylline group (67 premature deliveries), the perinatal death rate was 7.1%, compared to 17.9% in the control group (75 deliveries). Notably, the aminophylline group exhibited a significantly lower frequency of IRD, at 10%, compared to 29.5% in the control group for all premature infants. When considering the timing of ruptured membranes, the decrease in IRD frequency was particularly significant in infants born to mothers with ruptured membranes for more than 24 hours. No adverse effects were observed in mothers or infants due to aminophylline administration.
You can read the abstract of the article at https://www.ajog.org/article/0002-9378(79)90355-7/pdf.
Axelrod DM, Anglemyer AT, Sherman-levine SF, et al. Initial experience using aminophylline to improve renal dysfunction in the pediatric cardiovascular ICU. PediatrCrit Care Med. 2014;15(1):21-7.
Initial experience using aminophylline to improve renal dysfunction in the pediatric cardiovascular ICU
This single-center retrospective cohort study aimed to assess the impact of aminophylline administration on creatinine clearance and urine output in children with acute kidney injury in the cardiovascular ICU. In the study, 31 patients with congenital or acquired heart disease received aminophylline under pediatric nephrologist consultation. Over a 7-day period, serum creatinine levels decreased, estimated glomerular filtration rate increased, daily urine output improved, and fluid overload decreased, while no complications related to aminophylline were observed. These findings suggest that aminophylline therapy may enhance renal function and urine output in children with oliguric acute kidney injury in the cardiovascular ICU, and further prospective studies are needed to confirm these effects independently of other clinical interventions and to ensure safety.
You can read the full article at https://journals.lww.com/pccmjournal/fulltext/2014/01000/initial_experience_using_aminophylline_to_improve.4.aspx.
Bhatt GC, Gogia P, Bitzan M, Das RR. Theophylline and aminophylline for prevention of acute kidney injury in neonates and children: a systematic review. Arch Dis Child. 2019.
Theophylline and aminophylline for prevention of acute kidney injury in neonates and children: a systematic review
This systematic review and meta-analysis aimed to compare the effectiveness and safety of theophylline or aminophylline for preventing acute kidney injury (AKI) in neonates and children. The analysis included nine trials, with a focus on six trials involving 436 term neonates with severe birth asphyxia who received a single theophylline dose. The results demonstrated a 60% reduction in AKI incidence (moderate-quality evidence) and decreases in serum creatinine levels over days 2-5. There was no significant difference in all-cause mortality, and theophylline was associated with improved negative fluid balance, increased glomerular filtration rate (GFR), and decreased urinary β2 microglobulin. This suggests that a single prophylactic theophylline dose can help prevent AKI/severe renal dysfunction in term neonates with severe birth asphyxia without increasing complications or impacting mortality (very low-quality evidence).
You can read the abstract of the article at https://adc.bmj.com/content/104/7/670.long.
Djaladat H, Tajik P, Fard SA, Alehashemi S. The effect of aminophylline on renal colic: a randomized double blind controlled trial. South Med J. 2007;100(11):1081-4.
The effect of aminophylline on renal colic: a randomized double blind controlled trial
The study aimed to assess the effectiveness of aminophylline infusion as a pain reliever compared to a placebo in patients with acute renal colic. Over a study period from March to August 2005, 141 eligible patients were randomly assigned to receive either aminophylline or a placebo under double-blind conditions. Aminophylline proved effective in 64% of the patients, with a notable reduction in pain intensity 60 minutes after administration. In contrast, only 17% of the control patients receiving a placebo experienced pain relief. The study suggests that aminophylline can be a safe and cost-effective alternative to narcotic analgesics for managing renal colic, with minimal side effects and a potential to decrease the use of narcotics for pain relief.
You can read the full article at https://sma.org/southern-medical-journal/article/the-effect-of-aminophylline-on-renal-colic-a-randomized-double-blind-controlled-trial/.
Mcmahon K, Zappitelli M. Aminophylline for Acute Kidney Injury After Pediatric Cardiac Surgery: Finally Entering the Next Phase in Child Acute Kidney Injury Research. PediatrCrit Care Med. 2016;17(2):170-1.
Aminophylline for Acute Kidney Injury After Pediatric Cardiac Surgery: Finally Entering the Next Phase in Child Acute Kidney Injury Research
A recent study conducted by Axelrod et al. focused on assessing the impact of aminophylline in treating acute kidney injury (AKI) in children undergoing cardiac surgery with cardiopulmonary bypass. This single-center, double-blinded randomized clinical trial investigated the efficacy of aminophylline compared to a placebo and aimed to determine if it could reduce postoperative AKI. Despite the rationale for using aminophylline as it is a renal vasodilator and recommendations for its use in specific cases, the study did not find a significant reduction in AKI prevalence, raising concerns about the timing of intervention, among other factors. The study is seen as a significant step in AKI research but underscores the need for future studies that focus on AKI prevention rather than treatment.
You can read the abstract of the article at https://journals.lww.com/pccmjournal/fulltext/2016/02000/aminophylline_for_acute_kidney_injury_after.12.aspx.
Lynch BA, Gal P, Ransom JL, et al. Low-dose aminophylline for the treatment of neonatal non-oliguric renal failure-case series and review of the literature. J PediatrPharmacolTher. 2008;13(2):80–87. doi:10.5863/1551-6776-13.2.80.
Low-dose aminophylline for the treatment of neonatal non-oliguric renal failure-case series and review of the literature
The study aimed to evaluate the impact of low-dose aminophylline on renal function in neonates with acute renal failure. A retrospective review of 13 neonates who received aminophylline revealed that 77% of the patients experienced a resolution of acute renal failure, as evidenced by the normalization of serum creatinine and blood urea nitrogen. This suggests that low-dose aminophylline can be associated with an improvement in renal function indices in neonates with acute renal failure, even after other renal failure treatments have been attempted.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3462062/.
Mazkereth R, Laufer J, Jordan S, Pomerance JJ, Boichis H, Reichman B. Effects of theophylline on renal function in premature infants. Am J Perinatol. 1997;14(1):45-9.
Effects of theophylline on renal function in premature infants
A study assessed the impact of aminophylline on the developing kidneys of 19 premature infants with a mean gestational age of 31.1 weeks. It found that a 20-minute loading infusion of aminophylline induced significant diuresis and alterations in urinary excretion, including increased fractional excretion of sodium, potassium, calcium, and uric acid. These effects were transient and mostly disappeared within 24 hours, suggesting that the loading dose of aminophylline, but not the maintenance therapy, influenced renal function in premature infants. The study indicated that aminophylline primarily acts directly on tubular reabsorptive functions, as there were no significant changes in heart rate, blood pressure, or creatinine clearance.
You can read the full article at https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-2007-994095.
Mccullough PA, Larsen T, Brown JR. Theophylline or aminophylline for the prevention of contrast-induced acute kidney injury. Am J Kidney Dis. 2012;60(3):338-9.
Theophylline or aminophylline for the prevention of contrast-induced acute kidney injury
Caffeine and theophylline, natural methylxanthines, are recognized for their diuretic effects by blocking adenosine A1 receptors in proximal tubules and acting as renal vasodilators by counteracting adenosine-induced vascular constriction. However, they also stimulate renin secretion and disrupt renal adenosine balance. While theophylline has shown potential renoprotective effects in preclinical models after exposure to various stressors, the translation to clinical benefits in humans has been less convincing. Both aminophylline and theophylline have been used in the past to manage fluid overload in critically ill children before the advent of more potent diuretics.
You can read the abstract of the article at https://www.ajkd.org/article/S0272-6386(12)00943-2/fulltext.
Ix JH, Mcculloch CE, Chertow GM. Theophylline for the prevention of radiocontrast nephropathy: a meta-analysis. Nephrol Dial Transplant. 2004;19(11):2747-53.
Theophylline for the prevention of radiocontrast nephropathy: a meta-analysis
Background: Radiocontrast nephropathy, a common cause of acute renal failure in hospitalized patients, has seen several studies examining theophylline or aminophylline’s potential in preventing it, albeit with mixed findings. This meta-analysis of randomized controlled trials aimed to determine if administering theophylline or aminophylline before procedures could prevent radiocontrast-induced declines in kidney function. Seven qualifying trials (n = 480) were analyzed, revealing that the mean change in serum creatinine was 11.5 micromol/l lower in theophylline- or aminophylline-treated groups compared to controls, with only one participant (0.6%) requiring dialysis. The study suggests that prophylactic use of theophylline or aminophylline may safeguard against radiocontrast-induced kidney function declines, though their impact on patients with significant creatinine reductions or dialysis requirements remains unclear.
You can read the full article at https://academic.oup.com/ndt/article/19/11/2747/1809184?login=false.
Available from https://clinicaltrials.gov/ct2/show/NCT02983422.
Effects of Aminophylline on Renal Function and Urine Volume of AKI Patient
Acute kidney injury (AKI) is a sudden disruption of kidney function associated with high morbidity and mortality. Early diagnosis, aided by biomarkers, is crucial to apply informed interventions that can prevent irreversible kidney function loss. Adenosine, released within the injured kidney, constricts afferent arterioles, causing ischemic kidney injury. Aminophylline, converted to theophylline in the body, dilates afferent arterioles by blocking adenosine on the adenosine A1 receptor. Aminophylline and theophylline, nonselective adenosine receptor antagonists, have been effective in AKI management in various clinical scenarios. In a study involving patients above 18 years with AKI in the ICU, aminophylline was administered to the treatment group over 72 hours, while the control group received a placebo. This approach aims to explore the potential of aminophylline to mitigate AKI and its associated complications.
You can read the abstract of the article at https://classic.clinicaltrials.gov/ct2/show/NCT02983422..
Parker MR, Willatts SM. A pilot study to investigate the effects of an infusion of aminophylline on renal function following major abdominal surgery. Anaesthesia. 2001;56(7):670-5.
A pilot study to investigate the effects of an infusion of aminophylline on renal function following major abdominal surgery
Acute renal failure is a common complication in critically ill patients, and effective prevention remains a challenge. Some evidence from animal studies and limited human research suggests that aminophylline, through adenosine receptor antagonism, may mitigate renal damage in various conditions. In a study involving 20 post-surgery patients in an intensive care unit, intravenous aminophylline was administered without adverse cardiovascular effects. While there was a non-significant trend towards increased diuresis and improved renal sodium and osmolar clearance, creatinine clearance remained unchanged. The study was not designed to assess aminophylline’s impact on renal blood flow or glomerular filtration rate, indicating a need for further exploration of aminophylline’s renal effects in critical care settings.
You can read the full article at https://associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/full/10.1046/j.1365-2044.2001.01374.x?sid=nlm%3Apubmed.
Benoehr P, Krueth P, Bokemeyer C, Grenz A, Osswald H, Hartmann JT. Nephroprotection by theophylline in patients with cisplatin chemotherapy: a randomized, single-blinded, placebo-controlled trial. J Am Soc Nephrol. 2005;16(2):452-8.
Nephroprotection by theophylline in patients with cisplatin chemotherapy: a randomized, single-blinded, placebo-controlled trial
The study aimed to evaluate the potential of theophylline in preventing cisplatin-induced declines in glomerular filtration rate (GFR) among cancer patients. In a randomized, single-blinded, placebo-controlled trial, patients received cisplatin-based chemotherapy with or without theophylline. Those in the placebo group experienced a 21% reduction in GFR despite standard preventive measures, while theophylline recipients did not exhibit GFR deterioration. Theophylline was administered as an intravenous loading dose before chemotherapy, followed by oral maintenance. No adverse effects were reported during theophylline treatment, highlighting its potential to safeguard kidney function from cisplatin-induced damage.
You can read the full article at https://journals.lww.com/jasn/fulltext/2005/02000/nephroprotection_by_theophylline_in_patients_with.25.aspx.
Abizaid, A. S., Clark, C. E., Mintz, G. S., Dosa, S., Popma, J. J., Pichard, A. D., Satler, L. F., Harvey, M., Kent, K. M., & Leon, M. B. (1999). Effects of dopamine and aminophylline on contrast-induced acute renal failure after coronary angioplasty in patients with preexisting renal insufficiency. The American journal of cardiology, 83(2), 260–A5. https://doi.org/10.1016/s0002-9149(98)00833-9.
Effects of dopamine and aminophylline on contrast-induced acute renal failure after coronary angioplasty in patients with preexisting renal insufficiency
In the first phase of this study, 60 patients undergoing coronary angioplasty received saline, dopamine, or aminophylline, and the incidence of contrast-induced renal failure was 38%, with no significant difference among the three groups. In the second phase involving 72 patients with established contrast-induced renal failure, those receiving dopamine experienced worsened renal failure severity, leading to a prolonged course.
You can read the abstract of the article at https://www.ajconline.org/article/S0002-9149(98)00833-9/fulltext.
Barzegarnezhad, A., Firouzian, A., Emadi, S. A., Mousanejad, N., & Bakhshali, R. (2012). The effects of local administration of aminophylline on transureteral lithotripsy. Advances in urology, 2012, 727843. https://doi.org/10.1155/2012/727843.
The effects of local administration of aminophylline on transureteral lithotripsy
In a double-blind randomized clinical trial with 120 patients having ureteral stones, the effects of aminophylline on ureteral spasm during ureteroscopy for acute renal colic were investigated. The case group received a 250 mg dose of aminophylline in the irrigation solution, while the control group received saline. Ureteroscopy and transureteral lithotripsy (TUL) were performed five minutes after irrigation. The case group exhibited a shorter TUL duration (4.2 ± 2.61 min vs. 8.4 ± 2.9 min), a higher success rate (95% vs. 76.1%), and a lower need for extracorporeal shock wave lithotripsy (5% vs. 30%) compared to the control group, without significant post-TUL complications. Aminophylline improved the efficiency of ureteroscopy, reducing procedure duration, catheter requirements, stone migration, and the need for shock wave lithotripsy.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3469073/.
Seo, K., Choi, J. W., Kim, D. W., Han, D., Noh, S. J., & Jung, H. S. (2017). Aminophylline Effect on Renal Ischemia-Reperfusion Injury in Mice. Transplantation proceedings, 49(2), 358–365. https://doi.org/10.1016/j.transproceed.2016.11.043.
Aminophylline Effect on Renal Ischemia-Reperfusion Injury in Mice.
In this study on mice, aminophylline, known to increase intracellular cAMP levels and have anti-inflammatory effects, was examined for its impact on renal ischemia-reperfusion (I/R) injury. Mice were divided into three groups: a sham group (group S), a control group (group C) subjected to renal ischemia after nephrectomy, and an aminophylline group (group A) receiving aminophylline before ischemia. Aminophylline treatment resulted in significantly reduced serum creatinine, improved renal histology, and decreased expression of nuclear factor-kappa B (NF-kB), tumor necrosis factor-α (TNF-α), monocyte chemoattractant protein-1 (MCP-1), macrophage inflammatory protein-2 (MIP-2), and intercellular adhesion molecule-1 (ICAM-1) mRNA compared to the control group. These findings indicate that aminophylline provided renal protection against I/R injury, enhancing renal function and mitigating renal inflammation.
You can read the abstract of the article at https://www.sciencedirect.com/science/article/abs/pii/S0041134516309526?via%3Dihub.
Available from https://www.kireports.org/article/S2468-0249(22)00047-X/fulltext.
Sauer HE, Crews KR, Pauley JL, Bourque MS, Bragg AW, Triplett B, Morrison RR, Hall EA. Evaluation of Aminophylline for the Treatment of Acute Kidney Injury in Pediatric Hematology/Oncology Patients. J Pediatr Pharmacol Ther. 2021;26(5):484-490. doi: 10.5863/1551-6776-26.5.484. Epub 2021 Jun 28. PMID: 34239401; PMCID: PMC8244958.
Evaluation of Aminophylline for the Treatment of Acute Kidney Injury in Pediatric Hematology/Oncology Patients
This single-center, retrospective cohort study aimed to compare acute kidney injury (AKI)-related outcomes in pediatric patients who received aminophylline in addition to standard care with matched historical controls who received standard care alone. Patients treated for AKI from January 2017 to June 2018 were matched with historical controls from July 2015 to September 2016 based on age, sex, primary diagnosis, and hematopoietic cell transplant history. The primary outcome was the improvement in AKI stage at 5 and 10 days after treatment initiation. Results showed no significant difference in AKI resolution or the proportion of patients with resolved AKI when aminophylline was added to standard care in this pediatric hematology/oncology population.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8244958/.
Alsaadoun S, Rustom F, Hassan HA, Alkhurais H, Aloufi M, Alzahrani S, Bakhsh S, Dalbhi SA. Aminophylline for improving acute kidney injury in pediatric patients: A systematic review and meta-analysis. Int J Health Sci (Qassim). 2020 Nov-Dec;14(6):44-51. PMID: 33192231; PMCID: PMC7644458.
Aminophylline for improving acute kidney injury in pediatric patients: A systematic review and meta-analysis
This meta-analysis aimed to determine the effectiveness of aminophylline in pediatric acute kidney injury (AKI). A systematic search across six databases from January 1995 to May 2019 was conducted. Single-arm studies showed no significant changes in serum creatinine clearance, urine output, or blood urea nitrogen levels after aminophylline administration. In double-arm studies, aminophylline significantly reduced serum creatinine levels compared to the control group, but had no significant impact on AKI incidence, urine output, or mortality rates. Aminophylline appears to lower serum creatinine in pediatric AKI without adverse effects; however, further large-scale, well-designed trials are necessary to evaluate its efficacy and long-term effects.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7644458/.
Available from https://journals.lww.com/pccmjournal/Citation/2016/08000/Use_of_Aminophylline_to_Prevent_Acute_Kidney.26.aspx.
Use of Aminophylline to Prevent Acute Kidney Injury After Pediatric Cardiac Surgery
In a recent study published in Pediatric Critical Care Medicine, Axelrod et al. investigated the potential of aminophylline to prevent acute kidney injury (AKI) following pediatric cardiac surgery with cardiopulmonary bypass. While the authors made commendable efforts to control various factors influencing postoperative AKI, some essential aspects seemed insufficiently addressed. Notably, preoperative serum creatinine levels and preoperative use of angiography, which are known risk factors for postoperative AKI, were not provided. The study also omitted specific intraoperative risk factors affecting AKI in pediatric cardiac surgery, including mean arterial pressure fluctuations, deep hypothermic circulatory arrest, and medication usage. Additionally, the study didn’t present data on key variables like fluid overload and vasoactive inotrope scores, which are relevant for assessing AKI risk. Moreover, the study used a modified version of the KDIGO criteria, with variations in the time frame and a lack of consideration for urine output. These discrepancies may have affected the accuracy and interpretation of their findings.
You can read the full article at https://journals.lww.com/pccmjournal/fulltext/2016/08000/use_of_aminophylline_to_prevent_acute_kidney.26.aspx.
Bellos, I., Iliopoulos, D. C., & Perrea, D. N. (2019). Pharmacological interventions for the prevention of acute kidney injury after pediatric cardiac surgery: a network meta-analysis. Clinical and experimental nephrology, 23(6), 782–791. https://doi.org/10.1007/s10157-019-01706-9.
Pharmacological interventions for the prevention of acute kidney injury after pediatric cardiac surgery: a network meta-analysis
In pediatric patients undergoing congenital heart surgery, acute kidney injury is a significant concern. A meta-analysis was conducted to assess the efficacy of pharmacological interventions in preventing postoperative renal dysfunction. The analysis incorporated 14 studies with 2,625 patients and revealed that dexmedetomidine and acetaminophen significantly reduced the incidence of AKI, while corticosteroid, fenoldopam, and aminophylline showed no substantial benefit. Network meta-analysis indicated that dexmedetomidine had the highest likelihood of ranking first, albeit with some overlap with other treatments. This study emphasizes the need for more robust randomized controlled trials to establish the effectiveness of these interventions in safeguarding pediatric renal function during the perioperative period.
You can read the abstract of the article at https://link.springer.com/article/10.1007/s10157-019-01706-9.
Van den Eynde, J., Cloet, N., Van Lerberghe, R., Sá, M., Vlasselaers, D., Toelen, J., Verbakel, J. Y., Budts, W., Gewillig, M., Kutty, S., Pottel, H., & Mekahli, D. (2021). Strategies to Prevent Acute Kidney Injury after Pediatric Cardiac Surgery: A Network Meta-Analysis. Clinical journal of the American Society of Nephrology : CJASN, 16(10), 1480–1490. https://doi.org/10.2215/CJN.05800421.
Strategies to Prevent Acute Kidney Injury after Pediatric Cardiac Surgery: A Network Meta-Analysis
Pediatric cardiac surgery often leads to acute kidney injury (AKI), associated with increased morbidity and mortality. A comprehensive analysis of available preventive strategies for postoperative pediatric cardiac surgery-related AKI was conducted, encompassing 20 randomized controlled trials and 11 interventions. The study found no significant differences compared to control with corticosteroids, fenoldopam, hydroxyethyl starch, or remote ischemic preconditioning in traditional pairwise analysis. However, trial sequential analysis suggested an 80% relative risk reduction with dexmedetomidine and potential benefits from remote ischemic preconditioning. Network meta-analysis did not reveal significant differences among the examined treatments, including acetaminophen, aminophylline, levosimendan, milrinone, and normothermic cardiopulmonary bypass. While milrinone emerged as the most promising option, current evidence doesn’t strongly support any single strategy for pediatric AKI prevention.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8498996/.
Leow, E. H., Chan, Y. H., Ng, Y. H., Lim, J., Nakao, M., & Lee, J. H. (2018). Prevention of Acute Kidney Injury in Children Undergoing Cardiac Surgery: A Narrative Review. World journal for pediatric & congenital heart surgery, 9(1), 79–90. https://doi.org/10.1177/2150135117743211.
Prevention of Acute Kidney Injury in Children Undergoing Cardiac Surgery: A Narrative Review
Preventing acute kidney injury (AKI) in children undergoing cardiac surgery is crucial due to its association with elevated mortality and morbidity. Modifiable risk factors such as avoiding renal perfusion issues, nephrotoxic medications, and fluid overload can help reduce AKI risk. Although various pharmacological methods like aminophylline, dexmedetomidine, fenoldopam, and steroids have not shown strong evidence for routine use in AKI prevention, early peritoneal dialysis stands out as a robust nonpharmacologic approach for preventing cardiac surgery-associated AKI.
You can read the abstract of the article at https://journals.sagepub.com/doi/10.1177/2150135117743211?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Onder AM, Rosen D, Mullett C, Cottrell L, Kanosky S, Grossman OK, Iqbal HI, Seachrist E, Samsell L, Gustafson K, Rhodes L, Gustafson R. Comparison of Intraoperative Aminophylline Versus Furosemide in Treatment of Oliguria During Pediatric Cardiac Surgery. Pediatr Crit Care Med. 2016 Aug;17(8):753-63. doi: 10.1097/PCC.0000000000000834. PMID: 27355823; PMCID: PMC5515381.
Comparison of Intraoperative Aminophylline Versus Furosemide in Treatment of Oliguria During Pediatric Cardiac Surgery
A single-center, retrospective cohort study aimed to compare intraoperative aminophylline with furosemide for preventing or mitigating postoperative acute kidney injury (AKI) in pediatric congenital heart disease patients. While both groups had similar AKI incidence at 48 hours postoperatively, the aminophylline group exhibited more significant early postoperative urine production than the furosemide group. Notably, fewer children in the aminophylline group required renal replacement therapy compared to the furosemide group. These findings suggest that aminophylline may be more effective in reversing early postoperative oliguria and preventing AKI requiring renal replacement therapy. Future prospective studies on intraoperative aminophylline for cardiac surgery-associated AKI prevention are warranted.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5515381/.
Axelrod DM, Sutherland SM, Anglemyer A, Grimm PC, Roth SJ. A Double-Blinded, Randomized, Placebo-Controlled Clinical Trial of Aminophylline to Prevent Acute Kidney Injury in Children Following Congenital Heart Surgery With Cardiopulmonary Bypass. Pediatr Crit Care Med. 2016 Feb;17(2):135-43. doi: 10.1097/PCC.0000000000000612. PMID: 26669642; PMCID: PMC4740222.
A Double-Blinded, Randomized, Placebo-Controlled Clinical Trial of Aminophylline to Prevent Acute Kidney Injury in Children Following Congenital Heart Surgery With Cardiopulmonary Bypass
In a double-blinded, placebo-controlled, randomized clinical trial involving 144 children after congenital heart surgery with cardiopulmonary bypass, the study aimed to determine whether postoperative aminophylline administration could attenuate acute kidney injury (AKI). The results showed that aminophylline had no significant effect in preventing AKI in these children. There were no differences in the rate and severity of AKI, time to extubation, fluid balance, urine output, or other secondary outcome measures between the aminophylline and placebo groups. Aminophylline administration was found to be safe. Therefore, further investigation of preoperative aminophylline for AKI prevention in this patient population may be considered.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4740222/.
Saboute, M., Balasi, J., Tajalli, S., Hajipour, M., Heshmat, S., Khalesi, N., & Allahqoli, L. (2020). Effect of Aminophylline in Preventing Renal Dysfunction among Neonates with Prenatal Asphyxia: A Clinical Trial. Archives of Iranian medicine, 23(5), 312–318. https://doi.org/10.34172/aim.2020.20.
Effect of Aminophylline in Preventing Renal Dysfunction among Neonates with Prenatal Asphyxia: A Clinical Trial
In a randomized trial conducted in neonates with moderate to severe prenatal asphyxia, the effects of aminophylline on renal dysfunction were examined. Fifty-six neonates were randomly divided into two groups. The intervention group received a slow intravenous aminophylline injection (5mg/kg), while the placebo group received intravenous dextrose saline (2 mL/kg) during the first hour of life. Over the first and third days, the aminophylline-treated group showed significant improvements in creatinine levels, glomerular filtration rate (GFR), sodium levels, and urine output compared to the placebo group, indicating that aminophylline effectively prevented renal dysfunction in neonates with asphyxia.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/32383615/#:~:text=Conclusion%3A%20Aminophylline%20was%20effective%20in,the%20first%20day%20of%20life..
Available from https://ijp.mums.ac.ir/article_19738.html.
Chock, V. Y., Cho, S. H., & Frymoyer, A. (2021). Aminophylline for renal protection in neonatal hypoxic-ischemic encephalopathy in the era of therapeutic hypothermia. Pediatric research, 89(4), 974–980. https://doi.org/10.1038/s41390-020-0999-y.
Aminophylline for renal protection in neonatal hypoxic-ischemic encephalopathy in the era of therapeutic hypothermia
In a retrospective chart review of neonates undergoing hypothermia treatment for moderate/severe hypoxic-ischemic encephalopathy (HIE), this study assessed the impact of aminophylline on renal function. Sixteen neonates who received aminophylline showed increased urine output (UOP) and decreased serum creatinine (SCr) levels within 12 hours of treatment. When compared to a control group of cooled neonates without aminophylline, the UOP increase was more significant in the aminophylline group. While SCr decreased in survivors from both groups, baseline SCr was higher in the aminophylline group. This observational study suggests potential renal benefits of aminophylline, prompting the need for future randomized trials to confirm its role in neonates with HIE undergoing hypothermia.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7718287/.
Available from https://link.springer.com/article/10.1007/s00431-021-04128-6.
Kinbara, T., Hayano, T., Ohtani, N., Furutani, Y., Moritani, K., & Matsuzaki, M. (2010). Efficacy of N-acetylcysteine and aminophylline in preventing contrast-induced nephropathy. Journal of cardiology, 55(2), 174–179. https://doi.org/10.1016/j.jjcc.2009.10.006.
Efficacy of N-acetylcysteine and aminophylline in preventing contrast-induced nephropathy
In a study involving 45 patients undergoing coronary angiography (CAG) and/or percutaneous coronary intervention (PCI), the efficacy of N-acetylcysteine (NAC) and aminophylline in preventing contrast-induced nephropathy (CIN) was investigated. Patients were divided into three groups: NAC, aminophylline, and a control group receiving hydration only. The NAC group showed significant reductions in serum creatinine (SCr) and improvements in creatinine clearance (Ccr) after the procedure. In the aminophylline group, SCr and Ccr remained unchanged. In contrast, the control group experienced significant increases in SCr and decreased Ccr after CAG and/or PCI. The study indicates that both NAC and aminophylline effectively prevent CIN, surpassing the outcomes of hydration alone, suggesting their distinct mechanisms of action in countering CIN.
You can read the full article at https://www.journal-of-cardiology.com/article/S0914-5087(09)00280-9/fulltext.
Milani, L., Merkel, C., & Gatta, A. (1983). Renal effects of aminophylline in hepatic cirrhosis. European journal of clinical pharmacology, 24(6), 757–760. https://doi.org/10.1007/BF00607083.
Renal effects of aminophylline in hepatic cirrhosis
In 18 cirrhotic patients with impaired renal perfusion, the intravenous administration of aminophylline at 3 mg/kg body weight led to a significant increase in mean renal blood flow, from 1.77 to 1.99 ml/g/min (p < 0.01), without a notable change in cardiac output. In another 10 cirrhotic patients, aminophylline at the same dose reduced the mean tubular reabsorption of sodium in the proximal nephron section, resulting in an increase in free-water production due to greater sodium supply to the diluting segment. These findings demonstrate the favorable effects of aminophylline on renal functional impairment in hepatic cirrhosis.
You can read the abstract of the article at https://link.springer.com/article/10.1007/BF00607083.
- Available from https://scumj.journals.ekb.eg/article_54222.html.
Heidemann HT, Müller S, Mertins L, Stepan G, Hoffmann K, Ohnhaus EE. Effect of aminophylline on cisplatin nephrotoxicity in the rat. Br J Pharmacol. 1989 Jun;97(2):313-8. doi: 10.1111/j.1476-5381.1989.tb11956.x. PMID: 2758217; PMCID: PMC1854525.
Effect of aminophylline on cisplatin nephrotoxicity in the rat
The study investigated the impact of aminophylline, a methylxanthine compound, on cisplatin-induced acute renal failure in rats. Cisplatin caused polyuric acute renal failure with a significant reduction in creatinine clearance. Aminophylline ameliorated cisplatin-induced nephrotoxicity when administered during the maintenance phase of acute tubular necrosis but had no effect when given prophylactically before cisplatin application. In contrast, enprofylline, another methylxanthine without adenosine receptor antagonism, did not protect against cisplatin nephrotoxicity. These findings suggest a potential role of adenosine in the kidney’s hemodynamic changes induced by cisplatin.
You can read the abstract of the article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1854525/.
Rangel, M. O., Morales Demori, R., Voll, S. T., Wassouf, M., Dick, R., & Doukky, R. (2015). Severe chronic kidney disease as a predictor of benefit from aminophylline administration in patients undergoing regadenoson stress myocardial perfusion imaging: A substudy of the ASSUAGE and ASSUAGE-CKD trials. Journal of nuclear cardiology : official publication of the American Society of Nuclear Cardiology, 22(5), 1008–1018. https://doi.org/10.1007/s12350-014-0036-9.
Severe chronic kidney disease as a predictor of benefit from aminophylline administration in patients undergoing regadenoson stress myocardial perfusion imaging: A substudy of the ASSUAGE and ASSUAGE-CKD trials
The study examined the effects of aminophylline on regadenoson-induced adverse effects in patients with severe chronic kidney disease (CKD) using data from the ASSUAGE and ASSUAGE-CKD trials. Aminophylline showed a more significant reduction in gastrointestinal adverse effects (AE) in patients with severe CKD compared to those with better kidney function, with a notable absolute risk reduction (ARR) of 25% in the severe CKD group compared to 4% in the control group. This suggests that aminophylline administration provides an incremental benefit in reducing gastrointestinal AE in patients with severe CKD undergoing regadenoson stress myocardial perfusion imaging, making it a potential strategy to enhance their overall test experience.
You can read the abstract of the article at https://link.springer.com/article/10.1007/s12350-014-0036-9
Doukky, R., Rangel, M. O., Dick, R., Wassouf, M., Alqaid, A., & Margeta, B. (2013). Attenuation of the side effect profile of regadenoson: a randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease–the ASSUAGE-CKD trial. The international journal of cardiovascular imaging, 29(5), 1029–1037. https://doi.org/10.1007/s10554-012-0166-6.
Attenuation of the side effect profile of regadenoson: a randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease–the ASSUAGE-CKD trial
A subgroup analysis of the ASSUAGE trial revealed that standardized intravenous aminophylline administration after regadenoson-stress significantly reduces adverse effects in patients with severe chronic kidney disease (CKD). In a double-blinded, placebo-controlled trial with stage 4 and 5 CKD patients, 150 individuals received aminophylline, and 150 received a placebo. Aminophylline administration resulted in a 65% reduction in diarrhea, a 51% reduction in any regadenoson adverse effect, and a 70% reduction in headache. Patients in the aminophylline group showed better tolerance of the stress protocol. Importantly, the study found that ischemic burden remained similar between the two groups. In summary, standardized intravenous aminophylline administration substantially reduces the frequency and severity of regadenoson-stress-related adverse effects in severe CKD patients without altering ischemic burden.
You can read the abstract of the article at https://link.springer.com/article/10.1007/s10554-012-0166-6.
Olowu, W. A., & Adefehinti, O. (2012). Aminophylline improves urine flow rates but not survival in childhood oliguric/anuric acute kidney injury. Arab journal of nephrology and transplantation, 5(1), 35–39.
Aminophylline improves urine flow rates but not survival in childhood oliguric/anuric acute kidney injury
In this retrospective study, a group of Nigerian children with acute kidney injury (AKI) was treated with aminophylline, and their outcomes were compared to a control group. Both groups had similar baseline characteristics. Aminophylline-treated patients had significantly higher urine flow rates on days 5, 6, and 7, shorter duration of oliguria/anuria (6 days or less), and a reduced need for dialysis compared to the control group. However, there was no significant difference in mortality rates between the two groups. In summary, aminophylline therapy showed benefits in terms of improved urine flow and reduced dialysis requirements but did not significantly impact survival.
You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/22283864/#:~:text=Conclusion%3A%20Aminophylline%20therapy%20was%20beneficial,to%20impact%20positively%20on%20survival..
Mahaldar AR, Sampathkumar K, Raghuram AR, Kumar S, Ramakrishnan M, Mahaldar DA. Risk prediction of acute kidney injury in cardiac surgery and prevention using aminophylline. Indian J Nephrol. 2012 May;22(3):179-83. doi: 10.4103/0971-4065.98752. PMID: 23087551; PMCID: PMC3459520.
Risk prediction of acute kidney injury in cardiac surgery and prevention using aminophylline
In a prospective open-label trial, aminophylline was evaluated for its efficacy in preventing renal impairment after cardiac surgery in high-risk patients. Out of 138 patients undergoing cardiac surgery, 63 received aminophylline, while 75 received standard postoperative care. Patients with a Cleveland score of ≥6 had a higher incidence of acute kidney injury (AKI), with a number needed to treat (NNT) of 8, indicating that aminophylline infusion was associated with a reduced risk of renal function deterioration following cardiac surgery in high-risk individuals.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3459520/.
Shahbazi S, Alishahi P, Asadpour E. Evaluation of the Effect of Aminophylline in Reducing the Incidence of Acute Kidney Injury After Cardiac Surgery. Anesth Pain Med. 2017 Aug 27;7(4):e21740. doi: 10.5812/aapm.21740. PMID: 29696106; PMCID: PMC5903222.
Evaluation of the Effect of Aminophylline in Reducing the Incidence of Acute Kidney Injury After Cardiac Surgery
In an effort to reduce acute kidney injury (AKI) following cardiac surgery, this study administered aminophylline as an adenosine receptor antagonist to one group of patients undergoing surgery, while the control group received normal saline. The aminophylline group demonstrated earlier extubation (P = 0.018) and reduced inotropic drug use (P < 0.001). Using the RIFLE criteria, most patients in the aminophylline group experienced no change or even improvement in glomerular filtration rate (GFR) and creatinine (Cr) levels compared to the control group (p < 0.05). This suggests that aminophylline can reduce the frequency of AKI, making it a potentially effective and safe option for high-risk patients, also reducing the need for inotropic medication, length of stay in the intensive care unit, and extubation time.
You can read the full article at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5903222/.
Success Stories
 before after
before after
At the age of 60, I look and feel better than I ever have in my entire life! Switching my health program and hormone replacement therapy regimen over to Genemedics was one of the best decisions I’ve ever made in my life! Genemedics and Dr George have significantly improved my quality of life and also dramatically improved my overall health. I hav...
Nick Cassavetes ,60 yrs old
Movie Director (“The Notebook”, “John Q”, “Alpha Dog”), Actor and Writer
 Before After
Before After
I am now in my mid-sixties and feel better than I did in my 20’s. Many people have commented that I actually look 20 years younger since I started the program at Genemedics.
Calling Dr. George has proven to be one of the best decisions I have made in my life. Doctors and society convince us that developing various health issues and negative sy...
Pamela Hill ,66 yrs old
Call 800-277-4041 for a Free Consultation
- Usually takes 15-30 minutes
- Completely confidential
- No obligation to purchase anything
- We will discuss your symptoms along with your health and fitness goals
- Free post-consult access for any additional questions you may have
About
Genemedics® Health Institute is a global premier institute dedicated to revolutionizing health and medicine through healthy lifestyle education, guidance and accountability in harmony with functional medicine. Our physician-supervised health programs are personally customized to help you reach your health and fitness goals while looking and feeling better than ever.
Quick Links
Our Services
Our Locations
© Copyright Genemedics Health Institute. All Rights Reserved. Privacy Policy.